Toxic encephalopathy occurs as a result of long-term exposure to toxic substances, such as solvents, drugs, radiation, paints, industrial chemicals and certain metals.
The hallmark of encephalopathy is an altered mental state. Depending on the type and severity of the lesion, it is accompanied by various neurological symptoms - inability to concentrate, progressive loss of memory and cognitive abilities, subtle personality changes, lethargy. Other neurological symptoms may include involuntary twitching of one or a group of muscles (myoclonus), rapid involuntary movements of the eyeballs (nystagmus). Sometimes patients experience tremors, muscle atrophy and weakness, seizures, and loss of the ability to swallow or speak. One of the most severe consequences of brain damage is acquired dementia (dementia). Blood tests, cerebrospinal fluid examinations, brain imaging studies, electroencephalograms, and similar diagnostic tests may be used to determine the various causes of encephalopathy. Treatment is symptomatic and varies depending on the type and severity of brain damage.
Pathogenesis of the disease
Encephalopathy is not an independent disease, but a syndrome that reflects impaired functioning of the brain, spinal cord and even bone marrow. The pathological process is often caused by toxic damage to the body, among the provoking factors is chronic alcoholism. Under the influence of toxic substances, the structure and function of brain neurons are disrupted. In most clinical cases, this is an irreversible process. According to ICD-10, the code for this disease is G92.
This is what happens when alcohol toxic encephalopathy develops. Neurotoxins come from the environment or are released in the body due to poor functioning of the liver, kidneys, or endocrine system. Such toxic substances disrupt the integrity of neurons, causing them to die en masse. This is how single or multiple foci of necrosis are formed in the cerebral cortex.
More often, such “dead zones” provoked by hypoxic processes are localized in the cerebellum, brainstem or subcortical ganglia of the brain. The brainstem and diencephalic regions suffer from an acute lack of oxygen. Doctors do not rule out severe brain swelling as a complication.
Types of intoxication
There are two main types of intoxication in encephalopathy: chronic and acute. In the chronic form, a person will require long-term treatment. The body's strength is greatly depleted. They are no longer able to withstand constant intoxication. The chronic form appears in the later stages of the disease. As for the acute form, it occurs if a person is suddenly and severely poisoned by some toxic reagent. In this case, urgent medical care will help. assistance, as well as certain rehabilitation measures.
Acute and chronic form of the disease
The acute period of the disease does not last long and is accompanied by symptoms of severe poisoning. General health deteriorates sharply when a high concentration of poisons and toxins enters the body, after which the neurons die instantly. The clinical outcome depends on the concentration of harmful substances entering the body, the method of their influence on it, the timeliness and correctness of treatment.
More often, toxic encephalopathy in alcoholism is diagnosed in a chronic form. This is explained by the long-term intake of toxins into the body in relatively small and medium doses. As the poisons accumulate, they cross the blood-brain barrier and diffuse destruction occurs in neurons, with serious health complications.
Diagnostic measures
This disease is often diagnosed using a biochemical blood test. In addition, to clarify the diagnosis, a specialist can refer the patient to:
- Urine (urine) testing.
- Electroencephalography.
- Magnetic resonance imaging of the head.
The patient may deliberately not tell the doctor about the causes of toxic encephalopathy, not wanting to admit to using certain substances, which makes diagnosis very difficult. Also, a person may not know that he was exposed to toxic substances if he lived in an environmentally unfavorable place. In some cases, a patient may become intoxicated at a manufacturing plant where safety regulations were not followed and employees unknowingly put themselves at risk.
Causes of the pathological process
Before starting complex treatment of toxic encephalopathy, it is important to study the provoking factors. Otherwise, the prescribed therapy does not give the desired result, and the prognosis of the disease is less optimistic. Possible causes of encephalopathy:
- long-term alcohol abuse;
- drug use;
- inhalation of toxic substances;
- man-made accidents;
- interaction with household chemicals;
- taking illegal medications, including anesthesia and vaccinations.
Severe damage to the brain occurs when brain cells interact with the following toxic substances:
- petroleum products;
- pesticides;
- carbon disulfide;
- vapors of salts of heavy metals (lead, mercury, etc.);
- methyl alcohol, ethanol;
- carbon monoxide;
- nitrogen compounds.
In the absence of timely resuscitation measures for a long time, doctors do not rule out lifelong disability, or in complicated cases, the imminent death of the victim.
General symptoms of pathology
Signs of toxic brain damage are nonspecific, so timely diagnosis is sometimes difficult. In these cases, in order to make an accurate diagnosis, one has to wait until the full extent of the brain’s suffering develops. General symptoms of neuralgia:
- convulsive syndrome;
- numbness of a part of the body, limbs;
- migraines, frequent dizziness;
- signs of parkinsonism;
- panic attacks, nervous agitation;
- frequent attacks of nausea, severe vomiting;
- violation of cardiac detail;
- sudden weight loss;
- vegetative-vascular dystonia;
- impaired coordination of movements.
The attack begins with a stage of emotional upsurge. The patient behaves nervously and aggressively, does not control his actions, and is inadequate in speech and behavior. The effect of the toxin in the neurons gradually decreases, resulting in a state of stupefaction, the victim may fall into a coma or unconsciousness.
Symptoms of the disease depending on the provoking factor
If the cause of poisoning is lead or its compounds, the following signs of encephalopathy occur:
- heat;
- acute pain in the epigastric region;
- taste of a “copper coin” in the mouth;
- increased sweating;
- tachycardia;
- dyspnea;
- profuse vomiting.
In case of mercury poisoning, the following symptoms are added: hyperemia of the skin, tremors of the limbs, severe weakness throughout the body.
Separately, it is worth highlighting manganese toxic encephalopathy, which develops in a group of people whose work activities involve interaction with manganese compounds (industrialists, welders, miners). Consequences: high risk of Parkinson's disease. Manganese intoxication causes the following changes in the body and general condition of the victim:
- a sharp decrease in muscle tone;
- personality degradation;
- joint pain;
- severe weakness, body aches.
Symptoms of arsenic poisoning:
- severe headaches;
- white stripes on the nail plates;
- hair loss;
- peeling of the skin;
- weakness.
The symptoms of alcoholic encephalopathy are more extensive, which makes it easier to make an accurate diagnosis:
- digestive tract disorder;
- change in complexion, peeling of the skin;
- epileptic seizures;
- tremor of the limbs;
- cognitive impairment;
- alcoholic pseudoparalysis;
- Korsakov psychosis (incurable).
With alcohol intoxication and damage to the cerebral cortex, patients behave aggressively or are prone to depression. Hallucinations, panic attacks and obsessions are possible. The most dangerous in terms of severity is Gaye-Wernicke encephalopathy, which is accompanied by the death of the patient within 2 weeks.
Main clinical manifestations of toxic effects on the brain
Toxicological encephalopathy occurs differently in its acute and chronic forms. However, both neurotoxic processes usually occur with disruption of sensory and motor functions, emotional status, vision, and thinking abilities. In most cases, somatic pathology is added to the clinical picture.
Acute intoxication with neurotoxic poisons
Coma is a severe symptom of neurotoxic poisoning
Acute toxic encephalopathies often develop under the influence of synaptic poisons or substances that disrupt the conduction of nerve impulses along the nerve trunk. In this case, the effect of the xenobiotic can lead to inhibition or hyperactivation of nervous structures, as well as to the development of psychodysleptic conditions. In each of these cases, the signs of the disease will vary.
Inhibition of neurostructures leads to the appearance of the following symptoms:
- gait disturbance;
- dizziness;
- feeling tired;
- drowsiness;
- sopor;
- coma;
- cessation of spontaneous breathing.
The stimulating effect of some neurotoxic poisons leads to symptoms such as:
- excitation;
- convulsions;
- tremor;
- inadequate assessment of the surrounding reality.
Symptoms of psychodysleptic syndrome include:
- dizziness;
- hallucinations;
- rave;
- psychomotor agitation;
- feeling of euphoria;
- uncritical assessment of one’s own condition;
- inappropriate behavior.
Acute intoxication encephalopathy is usually accompanied by some somatic symptoms. Patients may experience numbness or pain in the extremities, inability to perform tasks requiring fine motor skills, and paresthesia.
Chronic intoxication with neurotoxic poisons
Outbursts of anger are one of the signs of chronic toxic encephalopathy
Toxic-metabolic encephalopathy of chronic course, as a rule, is of low specificity. Most known neurotoxic poisons, when administered in small doses for a long time, lead to the development of the same symptoms of the disease.
These include:
- irritability;
- depression;
- memory impairment;
- sleep disturbance;
- parkinsonism;
- extrapyramidal signs;
- mood swings;
- toxic encephalopolyneuropathy, which is often accompanied by behavioral disturbances and signs of peripheral neuropathy.
Encephalopathy during pregnancy
When carrying a fetus, there are 2 forms of the disease - physiological and pathological. In the first case, the disease is provoked by the instability of the emotional background of a pregnant woman. In the second - exposure to a strong toxin. Causes of pathological encephalopathy during pregnancy:
- late gestosis;
- toxic addiction;
- severe toxicosis;
- liver pathologies;
- atherosclerosis;
- injuries suffered during pregnancy;
- long-term vitamin deficiency.
An adult woman “in pregnancy” experiences internal fears and panic attacks due to the newborn baby and labor. Irritability appears in her behavior, and the fanatical instinct of self-preservation intensifies. The symptoms of encephalopathy during pregnancy do not end there:
- blood thickening;
- low blood pressure;
- vestibular disorders;
- drowsiness, general weakness;
- inhibition of reactions.
With the syndrome of cognitive impairment against the background of toxic encephalopathy, the patient degrades. Concentration, intellectual abilities and memory decrease. Based on such changes in behavior and thinking, one can also suspect the death of brain cells under the influence of toxins.
Diagnostics
At the first symptoms of encephalopathy, the patient urgently needs hospitalization and a comprehensive examination, which begins with collecting medical history data and examining the patient by a neurosurgeon. The main goal of diagnostics is to determine the type of toxin as quickly as possible and neutralize its effect in the body, restore the structure and functions of internal organs and systems. Recommended clinical examinations:
- Blood, urine, stool tests. Based on the results of laboratory tests, the degree of damage to the digestive tract, kidneys, liver, and other internal organs is determined.
- Electroencephalography. It is carried out in cases of severe convulsive syndrome and confusion to assess the degree of brain damage.
- Magnetic resonance imaging (MRI). The degree of brain damage is established, foci of necrosis and their parameters are visualized.
- Computed tomography (CT). An additional diagnostic method if MRI does not completely clarify the predominant clinical picture.
- Duplex scanning of cerebral vessels. The degree of reduction in blood flow through the vessels, the permeability of the walls and the narrowing of the lumen itself are revealed.
Toxic-metabolic and dismetabolic encephalopathy at any age are diagnosed in the same way. Depending on the causes of the pathological process, the intensive care regimen and clinical outcome change.
Complex treatment
When prescribing combination therapy, the following are taken into account: the degree of brain dysfunction, the type of toxin, and the stages of damage to internal organs. In case of exogenous (external) processes, the first step is to stop interacting with the neurotropic toxin. With endogenous influence (against the background of liver and kidney dysfunction), such a therapeutic measure is impossible. Therefore, it is necessary to carry out detoxification therapy, which includes:
- intravenous infusion of glucose and saline solutions;
- forced diuresis;
- gastric lavage;
- cleansing enemas;
- administration of an antidote;
- plasmapheresis;
- hemodialysis.
After cleansing the blood of toxic substances, symptomatic therapy is carried out for medical reasons. Recommendations depending on the patient’s condition in a particular case:
- For mental disorders and severe convulsive syndrome - tranquilizers, sedatives, magnesium sulfate, antipsychotics.
- For changes in tissue metabolism and cerebral circulation disorders - antihypoxants and vascular drugs (Cavinton, Cerebrolysin, Nootropil, Cinnarizine, Actovegin), vitamin therapy.
- To restore liver function - a monthly course of Essentiale Forte.
- For damage to the digestive tract in a complex treatment regimen - Limenda, Nolpaza, Pantoprazole.
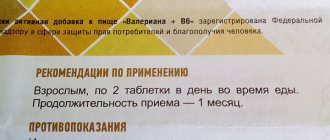
- To gently calm the nervous system - folk or sedatives (Motherwort).
- In case of encephalopathy, to speed up recovery, you need to take B vitamins in tablets, for example, Ferroplect, Neurobeks.
To speed up recovery, drug treatment is complemented by a course of physiotherapeutic procedures (10-15 sessions according to indications). Among them:
- acupuncture;
- water procedures;
- mud baths;
- head massage;
- physiotherapy;
- psycho-emotional therapy.
Preventive actions
To eliminate complications and consequences of toxic encephalopathy of the brain, timely preventive measures are important. First of all, you need to forever give up destructive habits - alcohol, toxic substances and dubious pills. Prevention is aimed at strengthening the body’s protective properties and normal functioning of internal organs and systems. Valuable recommendations from experts relate to the following aspects of human life:
- proper nutrition;
- walks in the open air;
- active lifestyle;
- playing sports;
- control of production and environmental factors;
- course vitamin therapy.
It is better to prevent the disease in a timely manner. In case of relapse, the patient’s chances of returning to a full life and being fully rehabilitated are negligible. The death of brain cells does not go away without leaving a trace. The degree of damage depends on the number and size of foci of necrosis and the timeliness of resuscitation measures.
Prevention
Rejection of bad habits
To reduce the risk of developing intoxication encephalopathy, it is necessary to minimize contact with toxins. You should stop taking drugs and alcohol. Any medications are used only as prescribed by a doctor. It is necessary to regularly undergo scheduled examinations and promptly treat diseases that can provoke severe intoxication of the body.
Consequences
Even after successfully completed treatment, the disease can recur. Potential health complications include:
- bleeding in the brain;
- polyneuropathy;
- asthenoneurotic syndrome;
- paralysis of limbs;
- speech disorders;
- schizophrenia, dementia;
- emotional instability, depression;
- visual and auditory hallucinations;
- Parkinson's disease;
- decreased potency in men;
- coma;
- stroke;
- death.
After a relapse, the functions of the peripheral nervous system are disrupted, and subsequent trophic disorders are accompanied by regular epileptic seizures.
Characteristic signs
Each manifestation of the disease has its own characteristics. They are caused by metabolic disorders, the manifestation of which is characteristic of an existing disease.
Hepatic encephalopathy
Its development provokes cirrhosis of the liver. The intensity of symptoms increases gradually. Initially, they manifest themselves in attention disorders, emotional disorders, judgments become inadequate, and memory becomes worse.
If you delay in seeking medical help, transient disturbances of consciousness may occur. It can fluctuate many times in one day, becoming either clear or confused.
A common symptom is the appearance of fluttering tremor, in other words asterixis. Sensitivity is impaired, which often happens with polyneuropathy, the pupils narrow, and reflexes intensify.
Uremic encephalopathy
The cause of uremic encephalopathy is renal failure. It is necessary to be wary if, for no apparent reason, a person becomes lethargic, apathetic, anxious, gets tired quickly, begins to perceive the surrounding reality more slowly, and becomes inattentive.
As the condition worsens, cognitive functions decrease and behavior does not always become adequate. The appearance of visual hallucinations and epileptic seizures is possible.
Neurological examination usually reveals muscle weakness and sensory disturbances. Such symptoms are accompanied by involuntary muscle twitching, instability while walking, fluttering tremors, and speech disorders.
Pancreatic encephalopathy
The reason for its appearance is acute pancreatitis or exacerbation of its chronic course. It starts suddenly. The appearance of hallucinations, convulsive movements, acute delirium (up to the occurrence of agitation), spastic paresis with paralysis is possible.
For diabetes
Encephalopathy is equally provoked by both hyperglycemia with ketoacidosis and hypoglycemia.
Ketoacidosis is characterized by disorders of consciousness in which epileptic seizures and focal neurological symptoms are absent.
Significant hyperglycemia is dangerous for impaired consciousness. Sometimes a state of increased drowsiness occurs, it is accompanied by:
- convulsions;
- neurogenic hyperventilation;
- delirium;
- disorders of consciousness.
Coma and epileptic seizures are not excluded. Bilateral loss of half of the visual field occurs, and convulsive movements appear.
For hyperthyroidism
Sleep deteriorates, absent-mindedness with irritability and emotional instability appears, attention becomes less concentrated. Depressive states, hallucinations, and, as an extreme case, psychosis with delirium are typical.
Forecast
Even with a timely response to a health problem, the prognosis for the patient is disappointing - lifelong disability. It is no longer possible to completely cure a person; their ability to work is partially or completely lost. In a patient with toxicological encephalopathy, intellectual abilities are permanently reduced, speech problems arise and intensify, and reactions are noticeably inhibited. The patient needs constant supervision.
Toxic encephalopathy is among the most dangerous diseases in neurology, since the destructive processes launched in the brain are fatal and irreversible. Without timely and emergency treatment, the affected person dies.
Other types of brain poisoning
Brain poisoning is caused not only by alcohol, but also by other toxic substances. Each intoxication is characterized by the presence of special symptoms.
| Toxin | Signs |
| Manganese |
|
| Mercury |
|
| Nicotine |
|
| Lead |
|
| Medicines |
|