Pneumonia itself is not a fatal disease; usually any of its forms occur with moderate or moderate severity.
Serious problems arise when a small child or an elderly person with a weak immune system gets pneumonia. In this case, the underlying disease is accompanied by pathological changes in the body. Pneumonia can worsen to the point of impaired consciousness, acute respiratory failure and other breathing problems. Detoxification therapy for pneumonia is the main method that effectively helps patients with severe pneumonia.
Symptoms of intoxication with pneumonia
Weakness, fever, increased sweating may be a sign of intoxication during pneumonia.
With pneumonia (pneumonia), intoxication appears as a result of the spread of infection through the lung tissues. This complication is accompanied by negative changes in some internal organs, as well as the nervous, cardiovascular and immune systems. The severity of intoxication is determined by the size and scale of the current inflammatory process. And also according to the occurrence of certain symptoms.
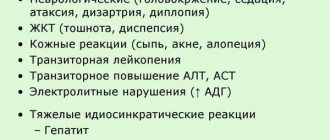
The main signs of intoxication during pneumonia are as follows:
- Weakness, noticeable loss of strength, lethargy.
- Prolonged increase in body temperature (within 38 degrees).
- Increased sweating.
- Noticeable weight loss of the patient.
[ads-pc-1] In case of moderate poisoning, additional symptoms occur:
- Nausea, frequent vomiting.
- Severe headaches, dizziness.
- A feeling of heaviness in the chest, a feeling of tightness.
- Difficulty breathing.
- Change in skin tone to grayish.
Severe poisoning is complicated by symptoms such as:
- Increase in body temperature to 39 degrees.
- More frequent and worsening vomiting.
- Increased duration and intensity of headaches.
If the patient does not receive the necessary medical care in a timely manner, his condition may quickly deteriorate. Then there is a possibility of convulsions and loss of consciousness. All this is fraught with serious complications. Prolonged poisoning of the body leads to the rapid development of anemia, so treatment should be started as soon as possible.
Consequences of complications
An incorrect approach to treatment or unauthorized discontinuation of medications can lead not only to the exacerbations described above, but also to other consequences:
- Chronic bronchitis is a pathology, the leading symptom of which is permanent coughing attacks, which are difficult to get rid of even with targeted treatment.
- Bronchial asthma is a chronic disease, as a result of which the bronchi spasm and secrete thick secretions that interfere with the normal respiratory process. Therefore, a person is forced to constantly use inhalers, which relieve bronchospasm for a short period of time.
- Fibrosis - if tissues are damaged during inflammation, the body can independently “repair” the damage with the help of special fibrous tissue. But if this tissue grows, the respiratory function is inhibited, which affects both the person’s well-being and the activity of all systems.
- Impaired activity of the liver and pancreas and dysbiosis are not a consequence of pneumonia and its complications, but of the medications taken. Antibiotics are necessary drugs for effective therapy, but, like any pharmacological agents, they carry health risks.
Symptoms of intoxication due to pneumonia in children
Young children do not have such a strong immune system as adults.
In children, intoxication due to pneumonia is especially difficult. Young patients are at high risk because they do not have such a strong immune system as adults, which would allow them to gradually cope with the disease.
Poisoning due to pneumonia in children is characterized by a staged development, which is characterized by the following stages:
1. Stage of general excitement. At this stage, all the internal organs and systems of the child work in active mode. Outwardly, this manifests itself as anxiety and nervousness. The following signs are noted:
- 1. Rapid heartbeat.
- 2. Frequent bowel movements (stool, most likely liquid), bladder.
- 3. Nausea, vomiting.
- 4. Restlessness, inability to sit still.
2. Suppression stage. At this stage, the activity of the baby’s organs and systems noticeably decreases. A stage begins, characterized by the child’s noticeable indifference to surrounding events. Sometimes stupor or “freezing” may occur. The baby's consciousness may also become clouded, drowsiness, and lethargy.
Poisoning of the body due to pneumonia in children has its own characteristics associated with the degree of dehydration:
The first degree is characterized by moderate thirst. There is slight dryness of the mucous membranes. The child is also likely to lose weight (up to 5%).
The second degree of dehydration is characterized by an increase in dry skin. The elasticity of tissues is also significantly reduced. A decrease in blood pressure and the appearance of tachycardia (rapid heart rate) are likely. The frequency of stool may also increase significantly (up to ten times a day), nausea and vomiting may occur. This degree is characterized by large weight loss (up to 9-10%).
The third degree of dehydration is accompanied by a serious increase in all of the above symptoms. The child has noticeably dry skin and mucous membranes, loose skin, shortness of breath, breathing problems, significant disturbances in the functioning of the digestive system, problems with heart rhythm, etc. Weight loss is more than 10%.
The last stage is considered dangerous and requires immediate hospitalization and quality medical treatment. If you do not start the required treatment procedures, there is a risk of death.
Symptoms
There is a direct relationship between somatic diseases and how the symptoms of congestive pneumonia manifest themselves. The underlying disease serves as a background against which congestion occurs in the lungs. Congestive pneumonia in the early stages is disguised as signs of the underlying disease.
The patient exhibits the following symptoms:
- wet cough with discharge of pus, mucus, and less often blood;
- prolonged increase in body temperature of the subfebrile type;
- excessive sweating;
- state of loss of strength, general lethargy, muscle weakness;
- difficulty breathing, a person feels that he cannot exhale completely.
It is quite problematic to detect the characteristic symptoms of the onset of congestion in the lungs.
Thus, with pathologies of the heart and blood vessels, symptoms will be characteristic, indicating the insufficiency of these organs. A stroke condition is primarily manifested by a malfunction of the lungs and changes in consciousness.
Against the background of symptoms of major somatic diseases, pleurisy develops with the release of fluid into the tissue (exudate) pericarditis. Breathing becomes weak and shallow, the skin takes on a yellowish tint. Tachycardia appears, heart sounds are muffled, the emphasis shifts to the second sound (aorta).
Breathing loses its normal rhythm and is manifested by the following phenomena:
- frequent shortness of breath;
- breathing rate increases sharply;
- tachycardia appears.
In older people with congestive pneumonia, there are signs of intoxication, which is accompanied by different temperature reactions of the body.
A depressed cough may be noted. The patient feels pain and heaviness in the chest and suffers from shortness of breath. When listening, pleural friction sounds and, less commonly, crepitus are detected. There is a dull tone in the lungs.
Extrapulmonary manifestations are characterized by elevated temperature. A person falls into a state of apathy, loses appetite, and becomes sleepy. There is a general state of lethargy, and involuntary urination appears.
The following diseases and pathological conditions can be the consequences of congestive pneumonia:
- swelling of the lungs;
- cardiopulmonary failure;
- toxic and infectious shock;
- death.
Basic elements of inpatient treatment of pneumonia
Patients with the acute stage of pneumonia are prescribed bed rest.
Patients with the acute stage of pneumonia are subject to mandatory hospital treatment. This is especially true for severe cases of the disease.
For the first few days, the patient is recommended bed rest, maximum rest, as well as careful qualified care from medical personnel. Constant medical supervision is required, since complications at this stage of the disease can arise very quickly.
The patient requires light nutrition, represented by the most fortified foods . Frequent drinking in large quantities is also a must.
If the patient is semi-conscious and his degree of illness is assessed as severe, then it is important to turn the patient over in bed from time to time. This is necessary to prevent possible congestion in the lungs, as well as to facilitate the discharge of sputum.
Antibacterial treatment is mandatory . If the pneumonia is at a fairly severe stage, the doctor prescribes the patient an intramuscular injection of semi-synthetic penicillins. These include the following drugs: methicillin, ampiox, etc. In addition to penicillins, the doctor prescribes simple sulfonamides. If after a few days there is an improvement in the patient’s condition (in particular, normalization of temperature), then antibiotic treatment is stopped.
To reduce signs of the inflammatory process, the patient is prescribed anti-inflammatory drugs . For example, small doses of acetylsalicylic acid. To eliminate DIC syndrome, the patient is prescribed intramuscular heparin.
Also, the patient is required to be given medications that promote expectoration and bronchodilators. If there is a pronounced rapid pulse (tachycardia), cardiotonic therapy is prescribed. As soon as the main signs of intoxication are eliminated, the patient is prescribed a complex of multivitamins.
In general, inpatient treatment of pneumonia and the consequences and complications of this disease is quite successful. Usually everything ends with the patient’s recovery. However, even after discharge, the patient needs to be observed for some time by a local therapist. It is also possible to be referred to physical therapy or a special course of physiotherapeutic procedures. This is necessary for the complete recovery of the patient and to prevent the protracted nature of pneumonia. [ads-pc-2]
Reasons for development
Failures in the functioning of the venous circulation in the pulmonary circulation lead to the emergence and development of hypostatic pneumonia. In this case, the respiratory organs suffer from failures of ventilation and drainage functions. As a result, the respiratory tract accumulates thick mucus - a suitable environment for the growth of pathogenic microflora. Most pathogens develop and accumulate in the lower parts of the right lung.
The pulmonary veins become passively overfilled, causing a decrease in blood outflow, the alveoli are compressed, and fluid leaks out of the bloodstream. The result of such changes is swelling followed by increasing pneumosclerosis with pleural effusion.
The likelihood of the disease occurring is much higher in older patients. Whose age has exceeded the sixty year mark. The risks become even higher in the presence of the following concomitant pathologies:
- diabetes mellitus;
- hypertension;
- heart defects;
- arrhythmias;
- ischemia;
- bronchial asthma;
- extrasystoles;
- pyelonephritis.
Hypostatic pneumonia develops not only in older people, but also in patients of other ages due to the prolonged passive position of bedridden patients. This category includes patients with bone injuries, postoperative patients, those who have suffered a stroke, cancer patients, severe forms of diabetes mellitus, traumatic brain injuries, and pathologies of the spine and chest.
Pneumonia appears both in the early (first days) stages of bed rest and in the later stages (up to six weeks).
The main pathogens are:
- pneumococci;
- streptococci;
- staphylococci and other pathogenic bacteria.
The presence of multiple somatic pathologies in elderly people leads to immobility in bed, the person is in a hypodynamic state, which contributes to the development of hypostatic pneumonia.
This kind of disease can also occur against the background of prolonged immobilization of patients after strip operations, wounds with circulatory disorders. In such situations, the lungs are not sufficiently ventilated, blood circulation reduces its intensity, and the body’s defenses are reduced due to the underlying disease.
Detoxification therapy for pneumonia - what it is, how it is carried out
In most cases, treatment of pneumonia is carried out inpatiently.
Detoxification therapy is the elimination from the body of toxic substances that provoked poisoning. For pneumonia, this therapy should be carried out in a hospital setting, since only there it is possible to provide the patient with bed rest, as well as the necessary nutrition. Also, in a hospital setting, intramuscular and intravenous administration of the required medications is possible. The implementation of therapy is constantly monitored by a qualified doctor, which guarantees a timely response to certain changes in the patient’s condition.
Diagnosis of the disease
Detection of the disease begins with a medical examination. Diagnosis is complicated by the presence of somatic symptoms in the patient. Doctors should not lose sight of the likelihood of developing congestive pneumonia in patients and monitor the general condition of the person.
Diagnostics is based on several methods:
- auscultation;
- X-ray examination of the lungs.
When listening, the hardness of breathing and the presence of wheezing, both dry and wet, finely bubbled, are determined.
X-ray shows a decrease in tissue transparency and an increase in the pattern of the lungs. An outline of the lesion or a line with a slightly expanding root may be detected.
The following examinations are also prescribed as diagnostic measures:
- Ultrasound of the pericardium and pleura;
- ECG;
- Echo-CG;
- blood sampling for general examination;
- blood chemistry;
- microscopy of sputum to identify cells affected by hemosiderin.
Goals and means of detoxification therapy
As a rule, detoxification therapy is carried out to achieve the following tasks:
- Ridding the patient's body of toxic substances of various kinds. During therapy, the patient is cleared of infectious agents, as well as their waste products. It also removes toxins accumulated in the body and interfering with the normal functioning of internal organs and systems.
- Normalization of water-salt balance, as well as electrolyte metabolism. Thanks to detoxification therapy, the patient’s water deficiency is replenished (if there was dehydration), and the blood is thinned. Its microcirculation also improves, and the functioning of all internal organs that were affected by poisoning is restored.
The means used are intramuscular and intravenous administration of the necessary drugs, as well as the use of all required accompanying medical procedures.
Detoxification Methods
In the process of implementing detoxification therapy, crystalloid and colloid solutions are used, as well as special products intended for parenteral nutrition.
Colloids are used to replenish fluid deficiency inside cells, as well as normalize water and electrolyte balance. These medications restore the required amount of blood, improve its microcirculation, and replenish the required amount of oxygen in the tissues. In addition, colloids stabilize metabolic processes in the body, improve the functioning of the lungs and other internal organs.
To provide parenteral nutrition to the patient, special solutions of vitamins and various microelements are used. In special emergency cases, combinations of these are used.
To treat intoxication in children, methods such as:
- Plasmapheresis. This method allows you to purify the blood of a small patient by removing its liquid part (plasma), which contains all the toxic substances.
- Hemodialysis. The blood is passed through a special hemodialysis membrane, where it is purified using the diffuse method.
In the practice of therapeutic departments, pneumonia is considered one of the most frequently diagnosed pulmonary diseases. More than 60% of the population suffer from various diseases of the respiratory system, which, when the immune system is weakened, are often complicated by pneumonia. At the Yusupov Hospital, great attention is paid to the treatment of the inflammatory process in the respiratory organs; treatment is carried out using modern methods using innovative medications.
Prevention measures
Prevention and implementation of mandatory recommendations is as follows:
- careful care of a bedridden patient;
- in bed it is necessary to periodically change the patient’s position independently or with outside help;
- breathing exercises;
- general massage, putting on mustard plasters, therapeutic exercises, placing the patient in a semi-sitting position;
- compliance with indoor air humidity and ventilation;
- if possible, the purchase and use of special orthopedic mattresses will reduce the likelihood of congestion in the lungs of a bedridden patient;
- regular monitoring by relatives (caregivers) at home of the patient’s breathing status;
- If wheezing or gurgling occurs when breathing, urgently
Call an ambulance.
The congestive form of pneumonia is dangerous and insidious. It requires timely detection and treatment. Otherwise, the consequences can be disastrous, even fatal. At the same time, it is possible to treat this disease, but strict adherence to the doctor’s prescriptions is required.
Removing Toxins
Detoxification is carried out not only in case of various poisonings, but also in the case of prolonged hypoxia. The procedure can also be prescribed if there is liver or kidney failure, pancreatitis, cystitis or gastritis. It is with such diseases that waste products of bacteria and viruses are released into the blood.
Types of medicines
To remove harmful substances, many solutions and preparations are used:
- Enterosorbents help get rid of toxins in the gastrointestinal tract. The most budget-friendly enterosorbents include Polysorb, which is perfect for use at home. The product is available in powder form. Enterosgel is also used. Both remedies can be taken not only when intoxicated, but also when living in an unfavorable environment.
- Infusion solutions, which are divided into crystalloid and colloid.
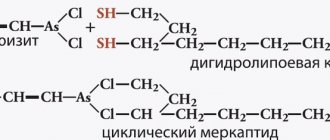
- Antidotes, that is, substances that are the opposite of the toxin, are used in cases of severe poisoning or infection. Each drug is selected after a thorough examination of the patient and tests that help determine what poisoned the person. For example, Dicaptol is used to remove arsenic.
- Laxatives speed up the removal of toxins from the body. In the hospital, castor oil and magnesium sulfate solution are used; at home, you can use various laxative drops and tablets.
conclusions
Complicated pneumonia can affect not only the bronchi and lungs, but also other organs and even the entire body. If pneumonia is not treated, what will happen? There will be bad consequences that will lead to the development of complications. Leads to death in 40% of patients.
Pneumonia is a very dangerous disease. Treatment of pneumonia should not be neglected under any circumstances; you should promptly seek help from a doctor.
Doctors recommend getting flu shots to avoid complications that lead to pneumonia. Don't smoke, don't drink alcohol, exercise, eat well and get plenty of rest. If doctors provide assistance on time, patients leave the hospital healthy. You need to monitor your health and consult a doctor on time.
The essence of the technique
In the case of all kinds of poisoning, when providing first emergency aid and stabilizing a person’s condition, an increased level of accumulation of toxic substances is noted in the tissues and internal systems of the body, in bones, joint and vascular tissue. They are the ones that should be removed in order to return the patient to good health.
Detoxification agents used during these procedures work to gradually cleanse internal systems, organs and resuscitate damaged cells.
Alcohol detoxification includes a large, carefully developed set of specialized measures that are aimed at quickly and safely relieving a severe hangover. This condition usually develops after excessive and prolonged consumption of alcoholic beverages.
Also, this technique becomes the basis when starting treatment of a patient for alcoholism. In addition, a timely cleansing procedure allows you to avoid the severe consequences of withdrawal symptoms and hangovers.
Various Ways to Detoxify
Depending on the condition of the human body, there are several methods of detoxification therapy. Drugs and various solutions are selected based on accumulated toxins.
Doctors highlight:
- Extracorporeal method.
- Intracorporeal treatment.
Features of extracorporeal therapy
This method is used only if it is not possible to remove toxic substances intracorporeally using detoxification agents.
There are several methods of cleansing the body:
- Dialysis, which requires a semi-permeable membrane, separates pure blood cells from toxic compounds.
- An apheresis procedure is performed using a centrifuge through which blood is passed. The purified blood remains in the human body, and all toxins are sent for further research to the laboratory.
- In case of severe intoxication, hemosorption is used. This procedure is carried out only when substances enter the body that can cause liver disease and cause irreversible damage to it.
- To reduce blood viscosity during drug or alcohol intoxication, ultraviolet irradiation is performed, which stimulates blood flow and improves the general condition of organs.
Intracorporeal detoxification method
This treatment is also called disinfection therapy, since it can be used to get rid of rare types of infections that arise after visiting exotic countries.
In order to remove toxic substances from the body, detoxifying agents are used, which are introduced into the bloodstream using a dropper.
Methodology used
As a rule, methods of detoxification for alcohol poisoning are based on the intravenous administration of a number of necessary drugs. Such as:
- in case of alcohol poisoning without pronounced symptoms of mental disorders, vitamin complexes Piracetam or Unitol are included in infusion therapy;
- if alcohol intoxication occurs against the background of various complications from the central nervous system, mental disorders, narcologists use antipsychotic medications (for example, Relanium or Tazepam).
Additionally, various means are used to stabilize night disorders, diuretics. All methods used for detoxification in alcoholism consist of a combination of several main techniques, in particular:
- Washing and cleansing the stomach.
- Infusion therapy (droppers).
- Therapeutic measures (symptomatic).
Gastric lavage (probing)
This measure is the best way to stop further absorption of poisonous and toxic residues of the metabolic products of ethyl alcohol into the internal systems. This procedure also works to reduce the load on the liver, stabilize it and, accordingly, significantly improve the functioning of the entire body.
How is alcoholism treated?
The simplest and most accessible method of gastric cleansing is the simultaneous intake of 2-3 tablespoons (large) of crushed activated carbon. The patient is then given a lot to drink and vomiting is induced. To do this, press on the root of the tongue.
When performing gastric intubation, narcologists often use subcutaneous administration of Apomorphine (0.2–0.5 ml of 1% solution).
After vomiting, the patient should rinse the throat and mouth thoroughly. Then, at the end of the lavage procedure, sodium bicarbonate (50 ml of a 4% solution) is injected into the gastric cavity using a probe. At the same time, the patient is given an aqueous solution of ammonia to drink (10–15 drops of ammonia are dissolved in 150 ml of water).
Carrying out infusion therapy
Droppers serve several purposes when cleansing the body of ethanol residues. Infusion therapy is aimed at:
- Blood purification.
- Stabilization of water balance.
- Regulation of electrolyte balance.
- Restoration of acid-base level.
This event is especially important and necessary if a person has acute alcohol poisoning (this situation has a high chance of developing into an alcoholic coma). The drugs used are selected by narcologists in accordance with the physiological characteristics of the patient and his current condition.
What is used in detoxification therapy
Intravenous infusion of a healing solution based on insulin, glucose, nicotinic and ascorbic acid helps to significantly alleviate the condition of the victim and reduce alcohol intoxication. Most often, droppers include:
- glucose;
- saline;
- ascorbic and nicotinic acid;
- Metadoxil (in combination with isotonic solution).
Metadoxil's work is aimed at accelerating the liver's production of a certain enzyme (alcohol dehydrogenase). This liver compound works to neutralize and remove alcohol residues from the body. Ultimately, this leads to increased oxidation and neutralization of ethanol metabolites.
All these measures taken together help to significantly reduce the severity of the syndrome and significantly reduce its duration. To restore water balance to normal, intravenous infusion of sodium chloride and glucose solution (isotonic) is used. Healthy electrolyte levels are stabilized by potassium chloride solution.
In the case of acute alcohol intoxication, infusion therapy often requires various additional measures (for example, ventilation, oxygen supply). Therefore, such treatment must be carried out in a hospital setting.
Symptomatic therapy
These measures are necessary when the narcologist is faced with the task of simultaneously providing the patient with detoxification measures the normal functioning of organic systems important for life. Such as:
- respiratory function;
- work of the nervous system;
- complete blood supply.
In case of observed disturbance of breathing processes, the patient is treated with analeptic drugs. In this situation, drugs such as Sulfocamphocaine or Caffeine are administered (subcutaneously). If these medications are ineffective, artificial ventilation of the lungs is performed.
If problems are observed in the functioning of the heart, cardiotropic medications (a group of cardiac glycosides) are added to treatment. Mildronate, Mtrofantine or Corglicon are often used. Caffeine is also used in case of a sharp drop in blood pressure. And for high blood pressure, Trental, Papaverine, No-shpu, magnesia or Eufillin are administered.
Diuretics such as Lasix or Mannitol can also be used. Many narcologists recommend including combined medications in infusion therapy (in the treatment of somatic disorders) that work to improve hemodetic processes.
How is symptomatic therapy carried out?
A rather important and necessary component for detoxification treatment is taking medications that work to restore and protect the liver. The most effective among these drugs are Heptral and Essentiale. These patients are also indicated for treatment using nootropics (for example, Piracetam) and ATP (sodium adenosine triphosphate).
It is very important for detoxification procedures to include medications based on vitamins C and B-group into therapy. These compounds work to restore redox reactions and carbohydrate metabolism. They also have a beneficial effect on the functioning of the respiratory and nervous systems and significantly improve the supply of oxygen to tissues.