The kidneys are a paired organ; they are located on the back under the 6th rib. The fact that a person has kidney pain and nausea is a common symptom of many pathologies.
Pain may be felt on only one side or on both sides at once. As a rule, they are localized in the back area near the spine near the last thoracic and first lumbar vertebra. Basically, pain in the kidneys spreads in the direction of the ureters to the external genitalia.
The nature of the pain is pulling, stabbing, cutting. They appear spontaneously, by palpation, when walking or playing sports. Pain can be triggered by changes in body position, alcohol consumption, colds, mechanical damage, and in women - menstruation and pregnancy.
It is important! Pain can make itself felt due to impaired blood flow in the kidneys, mental trauma, and severe fatigue. Thanks to this, blood rushes to the kidneys, so the organ begins to swell, squeezing the capsules and causing renal colic.
Urolithiasis disease
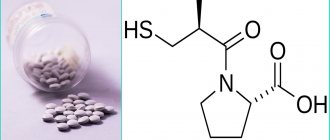
In urological practice, this condition is called urolithiasis. The formation of kidney stones occurs when calcium salts, uric acid crystals and other mineral salts accumulate in the renal pelvis.
The danger of this disease lies in the fact that full-fledged stones, when spontaneously moving, cause blockage of the ureter, which leads to the development of acute urinary retention. The advanced form of urolithiasis is characterized by renal intoxication, accompanied by acute pain, decreased daily diuresis or anuria, the appearance of a sallow skin color, nausea and vomiting.
Causes of nephritis
Pathology can be formed under the influence of the following factors:
- adverse effects of toxins, as well as their metabolic products;
- autoimmune reactions of the body observed in the affected areas.
Whatever the trigger, the pathology manifests itself in approximately the same way.
There is a dependence of the degree of damage to kidney cells on the percentage of toxins. The source of the poison and its chemical composition are also of great importance.
For the development of toxic nephropathy, sometimes minimal doses of toxic compounds are sufficient.
The development of the disease can occur under the influence of substances of biological and chemical origin. But more often you have to deal with the following sources:
- solvents of organic origin (acetic and oxalic acid);
- herbicides and pesticides;
- compounds of heavy metals and their salts (mercury, copper sulfate, lead, cadmium);
- long-term use of medications (sulfonamide drugs, aminoglycosides, ibuprofen and other non-steroidal anti-inflammatory drugs, anticoagulants);
- toxic compounds entering the body from the outside (poisons of inedible mushrooms; substances entering the bloodstream with insect bites; animal poisons);
- physical factors (injuries, electrical injuries, radiation sickness);
- volatile ethers (ethylene glycol, ethyl acrylate, dioxane);
- nitrogen-containing substances and their derivatives (arsenic, ammonia, nitrobenzene, aniline, hexachloroethane);
- surrogate alcoholic products;
- the result of an unsuccessful blood transfusion, sepsis (wrong group or Rh factor, blood poisoning).
Toxic nephropathy is a complex disease, the etiology of which can be different. This is why differential diagnosis is of utmost importance. If necessary, an antidote should be applied promptly.
Often cases of toxic damage to the body are associated with work in hazardous industries, where one regularly encounters toxic and chemical substances. The routes of entry into the body can be different:
- percutaneously;
- by airborne droplets;
- through the digestive system;
- through blood poisoning.
In addition, the development of the disease can be observed in the case of exotoxic shock, compression of the limbs or structural and functional disorders of the organ, as well as as a result of myoglobinuria (pathological breakdown of muscle protein with the presence of myoglobin in urine).
The development of the disease can also be a consequence of liver failure, when toxins that are not neutralized by the liver enter the blood, affecting other organs (heart, brain, kidneys).
The harmful effects of toxic substances lead to swelling of parenchymal tissues and failure of glomerular filtration, which, in turn, leads to impaired cell respiration and the gradual destruction of protein.
When the body is exposed to a hemotoxic poison (for example, after a snake bite), red blood cells are destroyed and nephrons are blocked.
Regardless of the method of intoxication, signs of oxygen starvation are observed in the renal tissue, followed by ischemia and necrosis of the renal tissue in the absence of timely treatment.
Pyelonephritis
Inflammatory damage to the renal pyelocaliceal apparatus occurs, as a rule, under the influence of an infectious factor. Other potential causes of this disease include traumatic kidney injuries, previous surgical interventions, as well as congenital or acquired abnormalities of the ureter structure.
Symptoms of renal intoxication with pyelonephritis do not have characteristic differences. Patients complain of severe nausea, vomiting, nagging pain in the lumbar region, discomfort and pain when urinating, general weakness and increased body temperature. Infectious pyelonephritis can be provoked by pathogens such as enterococci, staphylococci and E. coli.
Nephroptosis
This condition is characterized by a change in the anatomical position of the kidney due to its descent downwards. As a rule, the paired organ extends beyond its bed with a sudden significant loss of body weight, with regular weight lifting, as well as under the influence of other internal factors.
Most often, nephroptosis is diagnosed in young and middle-aged women who tend to indulge in various diets and therapeutic fasting. Very often, nephroptosis is formed under the influence of such factors:
- Long-term chronic constipation;
- Traumatic damage to the ligamentous apparatus fixing the kidney in the anatomical bed;
- Previously suffered rickets;
- Complications caused by pregnancy;
- Injuries of the lumbar spinal column.
Glomerulonephritis
This pathological condition is of an autoimmune nature and is characterized by severe damage to the renal glomeruli. In addition to the autoimmune factor, the development of glomerulonephritis can be caused by pathogenic microorganisms that penetrate the kidney through the ascending, hematogenous or lymphogenous route.
This severe pathological condition is accompanied by symptoms of renal intoxication, headache and dizziness, a decrease in the volume of daily diuresis or a complete absence of urine.
Along with the listed conditions, the causes of nausea and pain in the kidneys can be benign or malignant neoplasms in the area of the paired organ, as well as hydronephrosis, which is characterized by the accumulation of fluid inside the kidney, with its subsequent increase and the development of structural and functional failure.
Traditional recipes for pain
If pain develops in the kidneys and it is impossible to visit a doctor, you can try using folk remedies for pain.
These are herbal teas that are consumed instead of regular ones. Herbs such as motherwort, bearberry, cornflower petals, and licorice root have a good effect on the functioning of the organ.
The listed herbs are mixed in three tablespoons each and 300 ml of boiling water is poured. This tasty and healthy drink will significantly improve the patient’s health and well-being.
Kidney intoxication
The causes of nausea and pain in the kidneys are not only the above conditions, but also the entry of toxic substances and poisons into the human systemic bloodstream. Often this condition occurs when using certain groups of drugs, which with their metabolites damage the parenchyma of the paired organ.
If we say literally that this is kidney intoxication, then this is a pathological condition, as a result of which structural changes occur in the tissues of the organ, with the subsequent development of its failure. The so-called toxic nephropathy is characterized by rapid development and increased danger to human life and health.
In the initial period of structural and functional changes, intoxication is not accompanied by clinical symptoms or has a mild clinical picture. As structural and functional changes progress, the symptoms of renal intoxication take on the following form:
- Dyspeptic disorders, manifested by nausea and vomiting.
- Swelling in the face, neck, upper and lower extremities. This symptom complex indicates the development of functional renal failure.
- Pain syndrome localized in the lumbar spine. In some cases, patients complain of nagging pain in the lower back, which radiates to the perineum, left, and lower abdomen.
- Urinary disorders, which manifest themselves in the form of changes in the color of urine, the appearance of a characteristic sediment, a decrease in the volume of daily urine output or a complete absence of urine.
- Asthenovegetative syndrome. With the development of renal intoxication of various origins, a person experiences psychomotor retardation, general weakness, suppressed appetite, and decreased performance.
- Signs of hyperkalemia. When the filtration function of the kidneys is impaired, there is an increase in the concentration of potassium in the systemic circulation, resulting in changes affecting the functioning of the cardiovascular system and skeletal muscles.
This condition manifests itself in the form of depressed heartbeat, muscle weakness and a decrease in cardiac output.
Symptoms of poisoning
The severity of kidney damage depends on the presence of chronic diseases, the type and dose of toxic substances, and methods of penetration into the body.
Main symptoms:
- weakness, lethargy;
- nausea, vomiting;
- swelling, puffiness;
- diuresis changes, up to anuria;
- Blood pressure increases, muscles and joints may ache, convulsions and arrhythmia may develop.
Uncontrollable vomiting is one of the manifestations of poisoning
The victims complain that their kidneys hurt after poisoning. The composition and quality of urine is impaired. It becomes cloudy, dark, the smell and quantity change, protein and red blood cells appear, as a result of a violation of the filtration ability of the nephron glomeruli.
Uremia develops: a sharp, unpleasant odor from the mouth appears, the tongue becomes dry and covered with a brownish coating, the skin becomes pale and dry. The patient falls into a lethargic state, the pupils narrow, react weakly to light, the intensity of breathing changes, coma and death may occur.
Treatment
Therapy of renal intoxication of various origins requires an integrated approach, therefore such patients are usually treated in a specialized hospital. A comprehensive plan of therapeutic measures for this condition includes the following points:
- Detoxification measures. This set of measures is aimed at accelerating the elimination of toxic and metabolic substances, the accumulation of which served as a factor in the occurrence of intoxication. The components of infusion therapy are Ringer's solution, 5% glucose solution, and isotonic sodium chloride solution.
- The technique of forced diuresis, which consists of performing infusion therapy with one of the above solutions, followed by taking diuretics.
- Exchange transfusion of whole blood or plasma.
- In severe cases, patients are prescribed hemodialysis.
- Symptomatic therapy, including taking antiemetic, antiarrhythmic, analgesic and antihistamine (antiallergic) drugs.
If, against the background of severe renal intoxication, a person has developed exotoxic shock, glucocorticosteroids such as Prednisolone or Hydrocortisone are used to eliminate its manifestations. If a serious condition was provoked by the influence of poisonous and toxic components on the human body, then specific antidotes are administered to him.
Diagnosis of the disease
A set of diagnostic measures, as a rule, is carried out after the patient has been admitted to the nephrology department with suspected severe damage to the renal structures as a result of intoxication of the body. The general clinical picture of the disease is revealed, taking into account the collected medical history and determining the source and degree of poisoning.
Next, the doctor resorts to the following diagnostic procedures:
- a set of general clinical measures (general analysis of urine and blood);
- biochemical blood test (level of acid-base balance, urea, creatinine, blood ions, electrolytes, etc.);
- measuring the number and volume of urination per day;
- ultrasound examination of the kidneys;
- plain radiograph with contrast;
- performing angiography if necessary (examination of renal vessels);
- pyelography with contrast;
- MRI or CT scan of the kidneys.
Toxic nephropathy is characterized by an increase in leukocytes and ESR levels; changes in the density of urine, detection of protein, casts, red blood cells, and nitrogenous components in it. The amount of urea, creatinine and potassium in the blood increases. The disease is also characterized by the development of anemia, thrombocytopenia, and leukocytosis.
Complications
Kidney intoxication of various origins is dangerous due to the complications it can cause. If a patient with a similar diagnosis is not provided with timely medical care, he may encounter the following complications:
- Development of DIC syndrome;
- Chronic renal failure;
- Exotoxic or septic shock;
- Renal failure;
- Arterial hypertension;
- Metabolic acidosis and hyperkalemia;
- Hypochloremic or uremic coma;
- Violation of cardiac conduction, which manifests itself in the form of arrhythmia and extrasystole.
What can a doctor do?
The doctor will first determine the cause of kidney failure and the stage of the disease. After which all necessary measures will be taken to treat and care for the patient.
Treatment of acute renal failure is aimed primarily at eliminating the cause that causes this condition. Measures are applicable to combat shock, dehydration, hemolysis, intoxication, etc. Patients with acute renal failure are transferred to the intensive care unit, where they receive the necessary assistance.
Treatment of chronic renal failure is inseparable from treatment of the kidney disease that led to kidney failure.