Occupational poisoning can occur at chemical plants. The most common cause of intoxication in the workplace is not a violation of safety regulations, but a large amount of toxic substances that accumulate in the body and do not bother it for a long time. Employees who have worked for many years at chemical plants often suffer from occupational diseases due to intoxication with toxic compounds.
Features of toxic substances
Occupational poisoning is a pathology that develops under the influence of industrial toxins. Poisons differ in structure and characteristics. They are organic or inorganic compounds. Hazardous substances can be in gaseous, liquid and solid states. In the latter case we are talking about toxic dust.
Compounds with a polytropic nature of action are considered especially dangerous. Such substances can affect not one internal organ, but several. They can immediately affect the stomach and respiratory organs. There is a classification of poisons according to the direction of action. Toxic compounds selectively affect organs and systems of the body. A group of neurotropics affects the brain, while hematoxic substances change the composition of the blood, hepatotropic substances affect the liver and nephrotoxic kidneys.
Intoxication with neurotropes
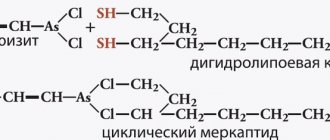
Chemicals have a detrimental effect on the nervous system. This group includes hydrocarbons, carbon disulfide, manganese, arsenic compounds, and metallic mercury.
Damage to the central nervous system also occurs as a result of contact with compounds that can cause dysfunction of internal organs.
These chemical compounds cause neurological disorders. Acute poisoning leads to loss of consciousness.
Occupational intoxication contributes to the accumulation of poisons. They depress the central nervous system gradually, resulting in mental disorders in people. It is difficult for an elderly person to cope with the consequences of such poisonings. After 60 years of age, he may develop Parkinson's disease or become unconscious.
Intoxication with hepatotropes
Chemicals damage the stomach and liver, and occupational types of poisoning are chronic. If an employee accidentally drinks poison, he can become poisoned instantly.
With this type of industrial intoxication, the liver is affected. If the root cause of the disease is not eliminated in time, toxic hepatopathy develops, which is the basis for hepatitis. The disease is treatable, and the person will get back on his feet and be cured partially or completely. It all depends on the severity and nature of the disease. It all depends on the severity of intoxication, the nature of the poisoning and the immune system of the poisoned person. The most dangerous chemical for cookies is lead.
Nephrotoxin poisoning
Occupational kidney and liver diseases may have similarities. They begin to develop after toxins that enter the human body are transported to these organs. Through the kidneys, toxic substances that cause the development of serious pathologies are removed from the body.
Dangerous compounds can slowly accumulate in the kidney structures and become causes of nephrological diseases.
How much damage the urinary system can suffer as a result of poisoning depends on what exactly caused the intoxication of the body. The causes of toxic nephropathy can be heavy metals, arsenic compounds or organic solvents. When the disease occurs, a person feels unwell and experiences pain in the kidney area.
Hematotoxin poisoning
Occupational diseases caused by intoxication can negatively affect the circulatory system. The clinical picture of the disease manifests itself in the following symptoms - anemia, leukopenia, problems with the hematopoietic organs. The danger of hematotoxins is that they release benzene compounds or other aromatic hydrocarbons that can cause severe harm to human health.
With this type of intoxication, hemoglobin changes and red blood cells are destroyed.
Dermatoses
A separate class of occupational intoxications includes dermatoses that appear on the skin upon contact with chemical compounds. Skin lesions can be caused by lubricating oils, acids, alkalis and other substances.
Occupational skin diseases eczema, angioedema, dermatitis, melasma and others are often caused by violations of safety regulations. You should not start work without taking care of personal protective equipment.
What are occupational diseases?
They are represented by various diseases that appear in a person as a result of working in harmful or dangerous conditions. This does not include overwork or deterioration of health due to long working shifts.
An injury sustained at work for various reasons is not an occupational disease. It is represented by a functional disorder that appears as a result of a citizen’s contact with various harmful or dangerous factors and substances. This contact must occur during the performance of work duties.
The management of different companies must apply different measures aimed at reducing harmful exposure to workers in order to reduce the number of occupational diseases. To do this, it is necessary to properly equip all workplaces with the necessary equipment and protective equipment.
Under what conditions can you get a work injury or occupational disease?
Conditions contributing to injuries and occupational diseases include:
- shortcomings in the organization of the work process;
- technical imperfection of production;
- non-compliance with sanitary and hygienic standards;
- socio-psychological negative factors;
- climatic features;
- characteristics of the specific personality of the employee (biographical reasons);
- economic conditions of production.
Eliminating (or at least reducing the negative impact on the work process) these conditions will help avoid or significantly reduce the likelihood of injuries and occupational diseases at work .
What could it be?
Occupational diseases can be presented in several types. These include:
- Chronic. It occurs when the human body is exposed to various harmful factors for a long time, such as loud noise, working with chemicals or other factors.
- Acute occupational disease. It lies in the fact that a person is influenced by various factors that lead to significant and rapid negative consequences for health.
Each incident at work must be thoroughly investigated in order to understand why a particular illness arose, what factors influenced its occurrence, and the investigation also reveals other important information.
For example, damage to the respiratory system that is detected in welders can be classified as a chronic disease, since they are constantly forced to work with various aerosols or other substances that contain aluminum, nickel, iron or other elements.
What is meant by acute occupational disease? This includes exposure to radiation on the human body for a short period of time. As a result of this process, the employee is diagnosed with radiation sickness, which leads to numerous negative consequences.
Types and categories of occupational diseases
In particular, we are talking about 5 groups of diseases of this kind, namely:
- 1 group. All diseases from this subgroup occur due to exposure to chemicals;
- Group 2 – diseases arise due to prolonged contact of the worker with dust;
- Group 3 – diseases associated with physical influences. For example, a noisy room or the influence of ultrasound, and so on;
- 4th group. Absolutely all types of diseases that belong to this group are associated with overexertion of the worker himself;
- Group 5 includes diseases due to exposure to biological factors.
It is worth noting that each group includes many diseases that employees of one or another production facility can get.
Features of the disease
Every employer should know what disease is called an acute occupational disease. It is quite easy to determine, since certain employee health problems should arise due to exposure to harmful factors over a short period of time. If such an impact is detected, it must be promptly eliminated. As a result, the employee faces the following negative consequences:
- temporary loss of ability to work, so sick leave is issued, after which the employer often offers easier working conditions;
- permanent loss of ability to work, as a result of which the citizen cannot continue to cope with work responsibilities, so he registers for a certain disability group and receives benefits.
Most often, an acute occupational disease leads to the fact that a company employee loses his ability to work. Often such effects on the body lead to the death of an employee. This is possible if during the performance of work duties he has to deal with dangerous factors.
Rehabilitation
After suffering stress, the body needs rest, which can be regarded as an important final stage of treatment. The main emphasis after poisoning in adults and children is on a light diet.
- On the first day, the patient must fast. Only heavy drinking is allowed. At the end of the day, if there are signs of improvement, you can give a tablespoon of rice water diluted in 1 liter of water.
- From the second day, a 2-week diet begins. You are allowed to eat little by little, in small portions, and only with light food. What you can eat: slimy decoctions and liquid porridges in water, vegetable puree soups, crackers.
Then it is gradually allowed to introduce low-fat broths, grated chicken fillet, steamed meatballs, cutlets, and fish. 2 weeks after acute poisoning, you can eat fresh vegetables and fruits to provide the body with vitamins.
Fatty, fried, seasoned, salted, smoked, dairy, and flour products should be completely excluded for a month after poisoning. The ban also applies to alcohol, coffee, and soda.
Diet is an important step towards recovery for patients. It is designed to speed up the restoration of the gastrointestinal tract and provide the body with nutrients. Along with your diet, it will be useful to include probiotics.
Signs of acute occupational disease
There are certain signs by which such a disease is detected. They depend on the source of the lesion. Most often, workers at various enterprises have to deal with radiation or chemical exposure. They become the causes of acute occupational diseases.
Radiation sickness is often detected in employees of industrial enterprises. This is due to the fact that a person is constantly exposed to radiation during work. The result of such exposure depends on the duration of irradiation and the dose received. Even if a person is able to recover, he will still be faced with cancer after a certain period of time.
Hepatotropes
These industrial products have an adverse effect on the digestive system and liver. Most often, such occupational intoxication is chronic. However, acute forms also occur, for example, when harmful substances are ingested.
An overdose of hepatotropes is manifested by painful sensations in the liver area. With prolonged intoxication, hepatitis gradually develops.
The most dangerous thing for this organ is lead poisoning. Unfortunately, hepatitis cannot always be cured. A lot depends on the person’s condition and the duration of the disease.
Concept of the register of occupational diseases
The Ministry of Social Development has approved a special classifier of occupational illnesses. It contains information about the name of each disease, its code, the cause of its occurrence and the factors that lead to its occurrence.
All ailments are divided into several groups depending on different influences leading to the occurrence of the disease, which can be chronic or acute. These impacts include:
- physical working conditions that may affect workers’ ability to work;
- biological effects;
- significant physical activity, which leads to changes in the functions of organs;
- chemical influences, and these include not only radiation, but also poisoning.
This register is regularly updated with new chronic and acute occupational diseases.
List of diseases and their classification in order No. 417n as amended in 2020
Diseases associated with unfavorable working conditions are systematized in the order of the Ministry of Health and Social Development of Russia dated No. 417n in the list of occupational diseases . The list of occupational diseases for 2020 is presented in 4 sections, each of which is compiled depending on the impact of adverse factors on a person.
These are the sections:
- Diseases (including poisoning) caused by chemical influence.
- Diseases caused by exposure to physical industrial causes.
- Diseases arising due to the influence of unfavorable biological factors.
- Diseases caused by physical exertion and functional overstrain of any organs or systems.
The list of occupational diseases in each section is presented as a list of diseases indicating the disease code, the name of the harmful factor, and the external cause code.
Types of occupational illnesses
Industrial managers must understand what is meant by an acute occupational disease, how an investigation is conducted, and what payments and benefits should be provided to employees.
Medical workers divide all diseases into two large groups:
- general ones that a person has until the moment he begins to perform work duties, but due to the influence of negative factors at work, the condition of the body worsens;
- professional, the causes of which are directly related to the work of a citizen.
It is in the second case that the employee can count on different types of help from the head of the company.
What disease is called acute poisoning, how does it differ from a chronic disease?
The concept of acute occupational disease (including acute poisoning) is also found in Resolution No. 967: this is the result of a one-time influence of a negative production factor on an employee.
Thus, acute poisoning (occupational disease) differs from a chronic disease in that it is characterized by:
- short-term (no longer than one working day or shift) influence of negative production factors on the human body;
- sudden onset;
- temporary (usually) damage to health, although in some cases it can be permanent.
How is the investigation carried out?
The procedure for establishing the presence of an acute occupational disease is to conduct a preliminary investigation. It is on the basis of this process that it is possible to determine whether a certain ailment discovered in a company employee is truly occupational.
During the investigation of acute occupational diseases, the participation of the following persons is required:
- local doctor or other employee of a medical institution;
- a representative of the Social Insurance Fund, since payments for accidents or professional illnesses are assigned specifically from this fund;
- other interested parties;
- administration of the specific enterprise in which the employee works.
An investigation is initiated by a direct employee of the company who is diagnosed with this disease. To do this, they perform the following actions:
- if any pain or other symptoms of illness are detected, you must immediately consult your doctor;
- all symptoms are listed, and the possible cause of the disease is explained;
- all working conditions in the company are described.
The remaining actions depend on the decision made by the attending physician.
First aid
In case of acute occupational poisoning at an enterprise, the victim must be taken away from the dangerous zone where the poison is spreading. Call an ambulance. While the medical team is on the way, monitor the condition of the poisoned person. Any further action must be taken depending on the employee’s well-being.
When the victim remains conscious, he is asked what is bothering him. It is necessary to measure and record pulse and blood pressure readings every 10 minutes. This allows you to track how the poisoning progresses. If the poisoned person is in a coma, you need to monitor how his heart works. If necessary, resuscitation measures must be performed. Do 15 chest compressions and 2 mouth-to-mouth breaths.
Attention! To perform artificial ventilation, you will need to take the victim into fresh air. Be sure to use a cloth napkin.
What should a doctor do?
Every doctor should know what disease is called an acute occupational disease or poisoning. Therefore, if the patient has the corresponding symptoms, the attending doctor must send a special notification to the state sanitary and epidemiological authorities. The specific form of the disease depends on the rate of progression:
- if serious symptoms are detected within 24 hours after exposure to certain factors at the place of work, then this form is acute;
- if the disease develops within three days, then its form is chronic.
Local manifestations of intoxication
Local are called manifestations in which the pathological process develops directly at the site of application of the poison. Possible local damage to the eyes, skin, respiratory tract and lungs, various
areas of the gastrointestinal tract. Local action can be manifested by alteration of tissues (formation of inflammatory-necrotic changes - the effect of acids and alkalis on the skin and mucous membranes; mustard gases, lewisite on the eyes, skin, mucous membranes of the gastrointestinal tract, lungs, etc.) and functional reactions (constriction of the pupil under the action of organophosphorus compounds on the organ of vision).
How is the organization verified?
Based on the application received from the doctor, an unscheduled inspection of the company by sanitary and epidemiological inspectors is carried out. The procedure for identifying an acute occupational disease is that specialists perform the following actions in the company:
- The employer is requested to provide a report containing the results of the assessment of employees’ jobs and other documents related to labor protection and the activities of the company’s employees;
- the situation that has arisen is analyzed, for which the workshop where the injured citizen worked is visited and inspected;
- a final act is drawn up.
The report, drawn up by sanitary and epidemiological inspection specialists, is sent to the medical institution where the company’s employee is being treated. The information received is studied by the management of this organization, after which a document is issued to the patient for signature. For reporting, a copy of this act is sent to the Social Insurance Fund and the employer.
Procedure and rules of registration
Registration and receipt of benefits is carried out in several stages, namely:
- Registration of the fact of receiving an occupational disease.
- Registration of the manual itself.
Registration of the fact of receiving an occupational disease
To obtain documentary evidence of the occurrence of an occupational disease, an employee must:
- Contact any medical facility. Based on the request, health workers notify the employer and the Social Insurance Fund about the possible presence of an occupational disease.
- Based on the notification, an inspection is carried out, where a corresponding act is drawn up.
- The drafted act is sent for approval to the Ministry of Health. The statement will mean that the victim has an occupational disease.
- Based on the report, the victim will be sent to the Center for Occupational Pathology, where an appropriate conclusion will be issued.
Documentation of benefits and benefits
It should immediately be noted that the Social Insurance Fund is responsible for .
Therefore, the injured party should:
- Contact your local physician at your place of residence.
- Upon application, the victim will be given a referral to undergo a full medical examination.
- After this, the therapist prepares the entire package of necessary documents and sends the victim to a commission (medical and social).
- Upon referral from the therapist, the commission confirms the fact that the injured party has an occupational disease, determines its degree and issues an appropriate documentary conclusion.
- With this conclusion, the injured party contacts the Social Insurance Fund and begins the procedure for obtaining benefits.
In addition to the conclusion itself, the victim must provide the following list of documents:
- original passport;
- act on the occurrence of occupational diseases;
- a copy of your work book, which confirms the fact of work in production;
- original certificate showing your average salary.
Based on the documents provided, a decision is made to provide financial assistance.
Occupational diseases at work are described in the following video:
Still have questions? Find out how to solve exactly your problem - call right now:
Didn't find the answer? Check out other materials
Conducting an investigation
As soon as it is proven that an employee has developed an acute or chronic occupational disease at the place of work, the company must conduct an investigation. Its main goal is to identify the causes of the disease, as well as the conditions for its occurrence.
A commission to investigate an acute occupational disease must be created. The head of the company can act as its chairman, and another official working in the company can also be selected. An employee is vested with the necessary powers as a result of the issuance of a corresponding order by the head. Additionally, the commission includes the chief physician of the hospital where the employee is being treated, a representative of the Social Insurance Fund and other government agencies.
The collegial body performs the following actions:
- all documents related to the work of the company are studied, but especially much attention is paid to documents related to labor protection at the enterprise;
- all working conditions in which the sick employee worked are studied;
- witnesses are interviewed;
- the premises where the victim worked are inspected;
- a final act is prepared, which specifies the conditions and causes of an acute occupational illness in an employee of the enterprise;
- the perpetrators, if any, are identified;
- Recommendations are drawn up for the company's management regarding eliminating the causes of occupational illness.
The head of the company is obliged to transfer to the commission all the necessary documents for study. It is even possible to request papers from the archives. The employer must provide any assistance to this collegial body, since it is in its interests to determine the cause of the occupational disease.
What documents are required?
To draw up a notice of an acute occupational disease, the commission must prepare a special investigation report. To do this, members of the collegial body study numerous documents requested from the employer. These include the following papers:
- characteristics of the victim’s workplace;
- an order on the basis of which a citizen gets a job;
- medical certificate containing information about the health status of the company employee;
- extracts from logs related to occupational health or safety, which must confirm that the employee has been instructed;
- special documents confirming that the citizen was issued personal protective equipment or other safety equipment;
- protocols of interviews with the direct victim, his colleagues, witnesses and responsible persons;
- medical expert opinions confirming that the employee actually has an acute occupational illness;
- other documents required by the commission members.
Based on all this documentation, an investigation report is drawn up. A copy of it must be kept in the company archive for at least 75 years, since it contains personal data about the company employee. It must contain the commission’s opinion as to who is to blame for the situation, what disease was discovered, and what measures will be taken by the company to prevent the occurrence of similar illnesses in other employees. It is determined whether the employee is at fault, and the information in the act must be agreed with the trade union.
If it turns out that a company employee is independently guilty of the situation, then he will not be able to receive benefits from the Social Insurance Fund.
What kind of benefit is provided?
An acute occupational disease is a serious and complex illness that leads to negative consequences for human health. It is often the cause of death of a company employee within the next 10 years.
When such an illness is detected, people partially or completely lose their ability to work, so they are assigned an appropriate benefit, paid from the funds of the Social Insurance Fund. Money is transferred through the employer. The size and types of payments depend on the citizen’s condition. The law does not provide for a specific list of payments and preferences, so they may differ slightly in different regions, since many benefits are offered by local authorities in different regions.
If an occupational illness occurs, the citizen is paid a one-time benefit, the maximum amount of which is 85 thousand rubles. Additionally, a monthly allowance is assigned, and its size depends on the citizen’s average earnings. A payment related to loss of ability to work is transferred at the place of work; otherwise, the maximum amount is 270 thousand rubles.
A person who has received an acute occupational disease, regardless of his age, can count on retirement. To do this, it is important that he has at least 9 years of experience, and the number of PF points must exceed 13.8.
Occupational diseases
Any employer is afraid of occupational diseases like fire - their recording, investigations, commissions, proceedings with the Social Insurance Fund, and increasing the insurance ratio. We, of course, feel very sorry for you, dear managers, but we still need to think about the employees and create favorable working conditions. And first of all, it is necessary to take care of employees in harmful, dangerous, heavy industries, where the risk of getting an occupational disease is especially high.
What is an occupational disease? This is a disease directly related to the work duties performed. The Labor Code of the Russian Federation talks about harmful and dangerous factors - features of your work that can lead to illness or injury (Article 209 of the Labor Code of the Russian Federation). Did you get a headache from the computer (once) or did the first signs of a cold appear from an unscrupulous colleague (why did you come if you were sick)? This is not an occupational disease, but an ordinary temporary illness. But if you feel a daily headache or constant malaise while at work, then you should consult a doctor. You may have developed symptoms of an occupational disease.
Treatment for poisoning
After diagnosis of acute poisoning, the patient will receive medical care. The main goal is to remove toxins and prevent complications for all body systems:
- gastric lavage through a tube,
- antidote therapy,
- restoration of intestinal flora,
- diuretics to remove poisons from the urine,
- laxatives,
- drips with the introduction of glucose solution and other drugs into a vein,
- normalization of enzyme activity,
- enema with administration of drugs,
- in difficult cases - blood and plasma purification, mechanical ventilation, oxygen therapy.
In parallel with the reduction in the concentration of toxins, the patient will undergo symptomatic treatment of acute poisoning (antipyretics to reduce pain or fever, sedatives in cases of overexcitation).
Curing severe poisoning is not an easy task. Sometimes it takes a lot of time and effort before the patient can feel healthy again.
Procedure for detecting an occupational disease
So, you still got sick. And you feel that this is not a one-time event, but a real professional disease. What do we have to do? First of all, go to the doctor.
There is an officially approved procedure for the employee and the employer in the event of detection of occupational diseases (RF RF No. 967 of December 15, 2000). The employee must take care of his health, confirm the professional nature of the illness and wait for compensation. The employer’s task is to correctly take into account the insured event, collect a commission, conduct an investigation, pay compensation to the employee and engage in professional prevention of occupational diseases. Here is the correct procedure for all parties involved in the incident:
- The employee goes to the doctor.
- The doctor orders tests, studies their results and makes a diagnosis.
- If an occupational disease is diagnosed, the medical specialist notifies the territorial body that controls occupational diseases - the center for state sanitary and epidemiological surveillance.
- The employer also receives notification from the attending physician.
- Specialists from the Center for State Sanitary and Epidemiological Surveillance are investigating the circumstances that led to the occupational disease. A sanitary and hygienic assessment of working conditions in the organization is being prepared.
- The conclusion is shown to the employer and the injured employee. If the parties do not agree with the resolution, they prepare written objections.
- At the same time, the doctor sends the employee for a full examination and finally diagnoses him with a disease resulting from professional activity. A special conclusion is being prepared based on the patient’s test results.
- If an employee is diagnosed with a chronic occupational disease, the attending physician sends him for an outpatient/inpatient examination within a month. This procedure is carried out in the center of pathology of occupational diseases. The patient must have in his hands all preliminary tests and extracts, information about medical examinations performed, an extract from the medical record, a sanitary and hygienic description of working conditions and a copy of the work record book.
- At the pathology center, they study the full history of the patient’s working life, check previous places of work for the possibility of exposure to dangerous and harmful factors, and make a final diagnosis - an acute or chronic occupational disease.
- At the same time, an investigation into the causes of occupational disease and an inspection of working conditions at the enterprise begins.
- The employer convenes a committee. The commission is headed by the chief physician of the center for state sanitary and epidemiological surveillance.
- Members of the commission collect the necessary materials, initiate examinations and laboratory tests, and conduct an independent assessment of the work at the victim’s workplace.
- After studying all the documents, the commission documents its conclusion. A special report on the case of occupational disease is drawn up.
- The employer fulfills all instructions from the act and notifies the center of state sanitary and epidemiological surveillance about preventive measures.
- The organization compensates the injured employee for the insured event.
Compensation for occupational diseases is paid to absolutely everyone - permanent (full-time) employees, external part-time workers, employees hired under the GPC, trainees, and seasonal workers. Individual entrepreneurs are also required to compensate their employees for cases of occupational diseases.
In other countries
But what is the situation with the recognition of COVID-19 as an occupational disease abroad?
Germany
The German list of occupational diseases mentions viral infections (No. 3101). It considers viruses as an occupational disease if the employee works in the healthcare sector.
But the virus is not considered an occupational disease for any other sector of the economy - such as public transport, supermarkets, construction, office workers, etc.
Italy
The National Institute of Work Accident Insurance (IstitutoNazionaleperl'AssicurazionecontrogliInfortunisulLavoro - INAIL) has confirmed that coronavirus infections of doctors, nurses and other employees of the National Health Service (ServizioSanitarioNazionale - SSN), as well as any other public or private health care institutions, are considered occupational diseases.
A causal link between work and infection will be automatically assumed for this group of workers to also cover cases in which identifying specific causes and modes of infection is problematic.
In addition, INAIL also covers cases where coronavirus infection occurred while traveling to work or back home.
Canada
Canadian Workers' Compensation Boards will compensate their workers for COVID-19 if:
- There is medical evidence that an employee who has been diagnosed with coronavirus (Covid-19) was exposed to SARS-CoV-2 in the workplace.
- This exposure was confirmed to be occupationally related.
Colombia
Coronavirus-19 is considered an occupational disease for healthcare workers and therefore entitles them to all existing sick leave benefits.
In addition to regular sickness benefits, workers diagnosed with Covid-19 have access to a temporary disability subsidy, cash benefit and funeral benefit.
France
Coronavirus is systematically and automatically recognized as an occupational disease for all carers, including those caring for their own workers. This includes full health coverage, increased daily benefits and increased protection associated with this type of risk.
Prevention of occupational diseases
The best prevention is maintaining proper working conditions. The employer is required to conduct annual medical examinations, purchase the correct (in accordance with industry regulations and standards) work equipment and personal protective equipment. Each employee must be familiarized (with signature!) with the working conditions at the enterprise, the level of harmful and dangerous factors and the list of possible occupational diseases that these factors cause. If production features entail potential risks, then the employer is obliged to reduce the level of harmfulness and danger, organize preventive measures, and control the work and rest schedules of employees.
The main task of the employer is not only to prevent employees from developing occupational diseases, but also to prevent them. It is important to constantly communicate with employees, find out about their health status (medical examinations, hello!), talk about possible deviations and necessary personal preventive measures. Preventive measures are systematic work, and not forced actions due to the occurrence of an insured event. If management regularly interacts with employees on labor safety issues and strictly follows legal standards, then there will be much less reason for inspections and investigations by regulatory authorities.
List of professions with hazardous working conditions
The list of professions with unfavorable labor conditions is defined in the Decree of the Government of the Russian Federation “On lists of work, production ...” dated No. 665. This document in its provisions makes reference to the lists of professions established by:
- Resolution of the USSR Cabinet of Ministers “On approval of lists...” dated No. 1173;
- Resolution of the USSR Cabinet of Ministers “On approval of lists...” dated No. 10.
Thus, current modern legislation confirms the legitimacy of regulations of the Soviet period.