This is a post-transfusion complication that occurs during massive transfusions of whole blood or plasma; metabolic reaction of the body to media prepared using sodium citric acid (sodium citrate). Clinically manifested by convulsive contractions of individual fibers of the lower leg muscles, coronary rhythm disturbances, pain or heaviness behind the sternum. Respiratory failure and tonic convulsions may develop. Diagnosed based on history, symptoms, and electrolyte test results. Treatment: cessation of transfusion, correction of metabolic disorders.
General information
Citrate intoxication (CI, post-transfusion hypocalcemia) is a relatively rare complication. Occurs in patients who need rapid and voluminous replenishment of blood volume using donor media. The occurrence does not exceed 0.01% of the total number of blood transfusions performed. It is diagnosed with equal frequency in men and women; about 60% of cases occur in patients over 50 years of age suffering from chronic kidney diseases and parathyroid glands. The phenomenon was described in the first third of the 20th century, shortly after sodium citrate began to be widely used as an anticoagulant and preservative.
First aid
If the patient has the symptoms described above, immediate action is necessary. It is very important to know how to relieve intoxication.
For any poisoning, the patient needs the following set of treatment measures:
- It is necessary to immediately hospitalize the victim in a medical facility.
- Provide the patient with detoxification aimed at removing toxic substances.
- Specific therapy is prescribed to suppress the poison.
- Symptomatic treatment is carried out.
Before the ambulance arrives, it is necessary to neutralize, if possible, the toxic effects of the poison. For these purposes, the stomach or skin is washed. It is acceptable to use a saline laxative. The patient can be given enterosorbents. The best drugs are “Activated carbon”, “Enterosgel”, “Sorbex”.
Causes
Citrate intoxication occurs with rapid transfusion of media that contain citric acid derivatives. Typically these transfusion media are plasma, whole blood or packed red blood cells. A drop in calcium levels to critical values occurs when the infusion rate is more than 100 drops per minute (1 liter in 10-12 minutes). Transfusion with a frequency of 150 drops has been proven to reduce the free Ca content to 0.6-0.8 mmol/l, with the average norm for an adult being 2.3-2.75 mmol. The likelihood of developing post-transfusion hypocalcemia increases in the following cases:
- Accompanying illnesses.
Utilization of sodium citrate occurs in the parenchyma of internal organs. Therefore, the complication is more common and more severe in patients suffering from liver cirrhosis, chronic renal failure, active hepatitis, and pancreatitis. Patients with multiple organ failure and shock of any origin require special caution during blood transfusion. - Taking corticosteroids.
Drugs such as prednisolone, dexamethasone, hydrocortisone, with long-term use, reduce the absorption of electrolytes from the gastrointestinal tract and increase their excretion through the kidneys. In addition, they lead to the leaching of microelements from bone tissue. Cytostatic agents have a similar effect. - Previous medical interventions.
Calcium concentration may change after replacement of the exfused volume with plasma, long-term hemodialysis, traumatic operations, and resuscitation measures. Sometimes procedures that can affect electrolyte levels are combined with the above diseases (hemodialysis due to renal failure). In such a situation, the risk of CI increases many times over.
Antidotes
Toxic poisoning must be treated with antidotes. They remove harmful substances from the body or neutralize them. These drugs are divided into types: antidotes with physical or chemical effects on toxins. Sorbents - unitopes - have a physical effect on poisons. There are serums that are classified as antidotes for immunological effects. Unitopes, serums and adsorbents are specific antidotes. The most common and accessible universal ones are:
- milk;
- clean drinking water;
- weakly brewed sweet tea;
- Activated carbon.
Pathogenesis
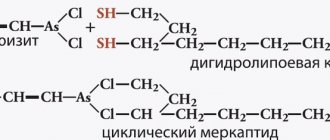
The pathogenesis is based on the ability of sodium citrate to bind Ca++ ions found in the blood plasma. Since this component takes part in electrophysiological processes, a lack of a microelement leads to their disruption. The stability of cell membranes is lost, the functioning of the sympathetic and parasympathetic nervous systems changes, the ability to regulate vascular tone decreases, and the synthesis of neurotransmitters and hormones fails. All this leads to the formation of a characteristic clinical picture.
The severity of CI is directly proportional to the volume and rate of citrated blood infusion. After the procedure is stopped, the electrolyte concentration is restored due to its release from intraosseous depots. Citric acid itself is quickly metabolized in the liver to inactive compounds. Minor and moderate intoxication does not require additional corrective measures. The functioning of all body systems is restored within half an hour from the moment the blood transfusion is stopped. In case of severe reactions, drug correction of calcium levels is indicated.
Food poisoning
Such intoxications are the most common. A big surge is observed in spring and summer. The air temperature rises during this period, which contributes to faster fermentation or souring of food.
Food poisoning is caused by eating spoiled or contaminated food. Poisonings can be bacterial or non-bacterial.
A person who has consumed low-quality food experiences the following symptoms:
- acute pain in the abdomen;
- nausea, vomiting;
- diarrhea;
- heat;
- chills;
- lack of appetite.
In severe cases, dysfunction of the kidneys, liver, and central nervous system is diagnosed.
Symptoms of citrate intoxication
At the initial stage, CI manifests itself mainly as subjective symptoms. Patients complain of discomfort in the chest and a metallic taste in the mouth. Slight shortness of breath may occur. As Ca concentration decreases, clinical manifestations increase. Convulsive contractions of individual muscle fibers of the face and legs appear. The breathing rate increases. There is a feeling of fear and drowsiness. There may be a headache, ringing in the ears, blurred vision, and a feeling of pins and needles on the skin. There is a decrease in blood pressure levels.
Severe hypocalcemia is manifested by tonic, long-lasting cramps, mainly affecting the muscles of the extremities. Vascular tone is noticeably reduced, which leads to severe hypotension. Shortness of breath increases, episodes of apnea appear. The heart rate drops, in the most severe cases asystole and clinical death develop. CVP and pressure in the pulmonary artery increases. The latter leads to swelling of the legs and accumulation of free fluid in the abdomen (ascites).
Complications
The most dangerous complication of CI is prolongation of the QT interval on the electrocardiogram. This phenomenon is considered a predictor of fatal arrhythmias and often ends in cardiac arrest or ventricular fibrillation. It occurs in almost all cases of excessive intake of citrate into the bloodstream. In the absence of other provoking factors, it disappears soon after calcium levels are restored. At a high risk, asystole is eliminated by intravenous administration of calcium-containing drugs. Well amenable to correction.
Another complication, occurring mainly in pediatric patients, is broncho- and laryngospasm. A picture similar to that of bronchial asthma is determined: expiratory dyspnea (with laryngospasm - inspiratory or mixed), a feeling of suffocation, lack of air, decreased saturation, generalized cyanosis. If the patient is able to sit, he takes a forced position, leaning forward and resting on his hands. A barking cough appears.
How to return to normal life?
When the main course of therapy is completed and the sick leave is closed, the person quite often continues to experience loss of appetite and weakness. There may be slight increases in temperature in the evening - these are the so-called temperature “tails”.
How to restore strength and alleviate the condition? The following recommendations may be taken into account:
- A course of multivitamins or simply a complete diet, balanced with all the main components of the daily menu: carbohydrates, fats and proteins, is useful. The diet must include the required amount of fruits and vegetables - sources of vitamins .
- During the fight against infection, the liver experiences a very high load. You can complete a course of restorative treatment with hepatoprotectors for a month. This group of herbal products reduces the effects of intoxication.
Fighting intoxication of the body, which causes deterioration in well-being and many unpleasant symptoms, correctly chosen antiviral therapy is the key to successful treatment and prevention of severe consequences, most dangerous for weak patients and children.
Diagnostics
Citrate intoxication is identified by characteristic clinical manifestations. The patient's medical history must include a recent transfusion of a large volume of transfusion media. Taking into account the fact that such procedures are most often carried out in the ICU or operating rooms, the patient is examined by an anesthesiologist-resuscitator. If necessary, a cardiologist or transfusiologist is consulted. To differentiate the condition from shock and allergic reactions, the following types of examination are indicated:
- Physical:
blood pressure is reduced by 20 or more units from the “working” indicators, the patient is scared, complains of heaviness in the chest, discomfort in the heart area, dizziness. The skin is pale or has a bluish tint, the respiratory rate is 22-25 per minute. With severe hypocalcemia, the respiratory rate is reduced to 5-10 times/min. There is evidence of hypertonicity of skeletal muscles and convulsive readiness. Contractions of individual fibers and twitching of facial tissues are visible. The pulse against the background of hypotension increases to 100-120 beats/min, but with a significant change in the salt balance it can decrease to 40-50 beats/min. - Instrumental:
the ECG reveals expansion of the ventricular complexes, an increase in the QT interval to 0.44 seconds or more. The RR interval increases to 1.2-1.3 seconds. at a recording speed of 25 mm/sec (bradycardia). The EEG shows changes in focal and asymmetric slow waves, indicating the presence of pathological brain activity. Measuring central venous pressure through a subclavian catheter reveals its increase to 15-16 mm of water column. - Laboratory:
the main method of examination is analysis of electrolyte content. In this case, the total Ca concentration decreases to the level
Treatment
The basis for eliminating the symptoms of hypocalcemia is immediate cessation of transfusion. If there are no significant disturbances in hemodynamics and muscle function, correction with medications is not indicated. The patient's condition returns to normal within a few minutes. If there is a significant change in the electrolyte balance and a clear clinical picture is present, the patient is intravenously injected with calcium chloride or gluconate in an amount of 10-20 ml of a 10% solution. Antidote therapy is not required because sodium citrate is quickly utilized in the body.
Citrate intoxication, which occurs in an extremely severe form, requires resuscitation. The patient is placed in the intensive care unit or intensive care unit, connected to an anesthesiological monitor for constant monitoring of the respiratory system and hemodynamics. In case of severe bradycardia, atropine and cardiotonics are administered. Generalized convulsions are relieved with Relanium, magnesium sulfate, and barbiturates. If a person is on mechanical ventilation, muscle relaxants in combination with hypnotics can be used for this purpose. The administration of calcium supplements under the control of blood electrolyte composition is indicated.
Prognosis and prevention
Citrate intoxication has a favorable prognosis if it is diagnosed in a timely manner. Stopping the transfusion or significantly reducing its rate allows the patient's condition to normalize even without the use of drugs. Severe hypocalcemia can cause fatal complications, including ventricular fibrillation or asystole, seizures, and respiratory failure or even respiratory arrest. The course of the disease worsens. There is a danger of developing post-hypoxic encephalopathy and other conditions associated with post-resuscitation changes.
Prevention consists of limiting the rate of transfusion of citrate-containing media. The infusion should be carried out at a frequency of approximately 50 ml/minute. People predisposed to the development of hypocalcemia are recommended to transfuse washed red blood cells that do not contain citric acid. If it is necessary to use citrate components, the patient should receive 10 ml of 10% Ca-gluconate for each liter of blood transfused. If the procedure must be carried out at high speed (critical conditions, acute blood loss), then the drugs are administered every 0.5 liters of transfusion medium.
It can develop with the rapid administration and transfusion of large quantities of canned blood. Sodium citrate (sodium citrate) is a common stabilizing agent for transfusions of both freshly citrated and preserved blood. Citrate introduced into the body is quickly destroyed and excreted, and with slow drip transfusions no complications are observed. However, with rapid (jet) transfusion of large doses of canned blood, nitrate intoxication may occur. The pathogenesis is based on the direct toxic effect of the preservative sodium citrate, as well as changes in the blood content of potassium and calcium ions. An increase in potassium concentration in transfused blood may be associated with increased hemolysis that occurs during long periods of storage. Sodium citrate is capable of binding calcium ions in the recipient's blood, thereby leading to hypocalcemia. A dangerous dose for the occurrence of citrate intoxication, especially in patients with liver and kidney diseases, is 10 mg⋅kg⋅min. Thus, when transfusing a patient weighing 70 kg with a stream of 150-200 ml of canned blood in 1 minute, there is almost always the possibility of nitrate intoxication (Permyakov P.K., 1985).
Clinically, severe nitrate intoxication manifests itself during or towards the end of transfusion in the form of collantoid reactions caused by weakened contractility and disturbances in myocardial conduction, up to cardiac arrest. These disorders are associated primarily with an imbalance of electrolytes (hyperkalemia, hypocalcemia) in the recipient’s blood. Suspicion of the occurrence of nitrate intoxication arises from some indirect signs; with the development of a collantoid reaction during or immediately after the administration of blood in the absence of clinical and morphological signs characteristic of other blood transfusion conflicts; in the presence of underlying liver disease and nights that metabolize and excrete citric acid salts.
The pathological picture is largely nonspecific. However, the study of cadaveric blood to determine the calcium content in plasma is quite specific. Determining the potassium content in cadaveric blood plasma is hardly worth recommending, since in cadaveric blood it is always elevated due to post-mortem hemolysis. Macroscopically, there is usually pronounced venous congestion, and the postmortem CVP is high. Hemorrhages in the serous and mucous membranes may occur.
Today, medical practice cannot be imagined without blood transfusions. There are many indications for this procedure, the main goal is to restore the lost blood volume to the patient, which is necessary for the normal functioning of the body. Despite the fact that it belongs to the category of vital manipulations, doctors try not to resort to it for as long as possible. The reason is that complications during transfusion of blood and its components are common, the consequences of which for the body can be very serious.
The main indication for blood transfusion is acute blood loss - a condition when the patient loses more than 30% of his blood volume in a few hours. This procedure is also used if there is unstoppable bleeding, a state of shock, anemia, hematological, purulent-septic diseases, or massive surgical interventions.
The blood infusion stabilizes the patient, and the recovery process after a blood transfusion is much faster.
Hemostasis disorders. DIC - syndrome.
In patients who have suffered massive blood loss and received transfusions of large volumes of blood, in 20–25% of cases various hemostasis disorders are established, the origin of which is due to the “dilution” of the patient’s plasma coagulation factors, hemodilution thrombocytopenia, the development of disseminated intravascular coagulation and, much less frequently, hypocalcemia. DIC syndrome plays a decisive role in the development of true posthemorrhagic and posttraumatic coagulopathy
Already after 48 hours of storage of donor blood, a significant decrease in the content of plasma blood coagulation factors is found in it, and after a few hours of blood storage, the hemostatic activity of platelets sharply decreases (such platelets become inactive). Transfusion of large quantities of canned blood with similar hemostatic characteristics in combination with the loss of the patient’s own blood leads to the development of disseminated intravascular coagulation syndrome. If a patient has massive blood loss (more than 30% of the initial bcc), transfusion of one volume of circulating blood reduces the concentration of plasma coagulation factors in the patient to 18–37% of the initial level. In patients with disseminated intravascular coagulation syndrome due to massive transfusions, diffuse bleeding from surgical wounds and from injection (puncture) wounds is observed. The severity of the manifestations of DIC syndrome depends on the amount of blood loss and the required volume of transfused transfusion media, correlated with the recipient's BCC.
Treatment of patients with DIC syndrome
due to massive transfusions, it is based on replenishment of missing coagulation factors. The best transfusion media for replenishing the missing components of the hemostatic system are fresh frozen plasma and platelet concentrate.
Fresh frozen plasma is preferable to cryoprecipitate because it contains the optimal range of plasma coagulation factors and anticoagulants. Cryoprecipitate may be used if it is suspected that the main cause of impaired hemostasis is a marked decrease in fibrinogen levels. Transfusion of platelet concentrate in this case is certainly indicated when the platelet level in patients decreases below 50 x 10 9 /l. The cessation of bleeding is observed when the platelet level increases to 100 x 10 9 /l. If massive transfusion is necessary, the possibility of developing massive transfusion syndrome must be anticipated. If the blood loss is severe and transfusion of large quantities of red blood cells, saline solutions and colloids is necessary, then platelet concentrate and fresh frozen plasma should be prescribed before the development of hypocoagulation. They recommend transfusion of 200 - 300 x 10 9 platelets (4 - 5 units of platelet concentrate) and 500 ml of fresh frozen plasma for every 1.0 liter of red blood cells or suspension transfused (in conditions of replenishment of acute massive blood loss).
Post-transfusion complications
Post-transfusion complications during transfusion of blood and its components are common; this procedure is very risky and requires careful preparation. Side effects arise due to non-compliance with the rules of blood transfusion, as well as individual intolerance.
All complications are divided into two groups. The first includes a pyrogenic reaction, citrate and potassium intoxication, anaphylaxis, bacterial shock, and allergies. The second includes pathologies caused by incompatibility between the donor and recipient groups, such as blood transfusion shock, respiratory distress syndrome, renal failure, and coagulopathy.
Allergic reaction
Allergic reactions are the most common after blood transfusion. They are characterized by the following symptoms:
- skin rash;
- attacks of suffocation;
- Quincke's edema;
- nausea;
- vomit.
Allergies are provoked by individual intolerance to one of the components or sensitization to plasma proteins infused earlier.
Pyrogenic reactions
A pyrogenic reaction may occur within half an hour after infusion of the drugs. The recipient develops general weakness, fever, chills, headache, and myalgia.
The cause of this complication is the ingress of pyrogenic substances along with transfused media; they appear due to improper preparation of systems for transfusion. The use of disposable kits significantly reduces these reactions.
Citrate and potassium intoxication
Citrate intoxication occurs due to exposure of the body to sodium citrate, which is a preservative for hematological drugs. Most often it manifests itself during jet injection. Symptoms of this pathology are a decrease in blood pressure, changes in the electrocardiogram, clonic convulsions, respiratory failure, even apnea.
Potassium intoxication occurs when a large volume of drugs is administered that have been stored for more than two weeks. During storage, potassium levels in transfusion media increase significantly. This condition is characterized by lethargy, possible nausea with vomiting, bradycardia with arrhythmia, up to cardiac arrest.
To prevent these complications, before massive blood transfusion, the patient needs to be administered a 10% calcium chloride solution. It is recommended to pour in ingredients that were prepared no more than ten days ago.
Blood transfusion shock
Hemotransfusion shock is an acute reaction to a blood transfusion that occurs due to incompatibility between the donor and recipient groups. Clinical symptoms of shock may occur immediately or within 10-20 minutes after the start of the infusion.
This condition is characterized by arterial hypotension, tachycardia, shortness of breath, agitation, redness of the skin, and lower back pain. Post-transfusion complications during blood transfusion also affect the organs of the cardiovascular system: acute expansion of the heart, myocardial infarction, cardiac arrest. Long-term consequences of such an infusion are renal failure, disseminated intravascular coagulation syndrome, jaundice, hepatomegaly, splenomegaly, and coagulopathy.
There are three degrees of shock as complications after blood transfusion:
- mild is characterized by low blood pressure up to 90 mm Hg. st;
- average: systolic pressure decreases to 80 mmHg. st;
- severe - blood pressure drops to 70 mm Hg. Art.
At the first signs of transfusion shock, the infusion should be stopped immediately and medical assistance should be provided.
Respiratory distress syndrome
The development of post-transfusion complications and their severity can be unpredictable, even threatening the patient’s life. One of the most dangerous is the development of respiratory distress syndrome. This condition is characterized by acute impairment of respiratory function.
The cause of the pathology may be the administration of incompatible drugs or non-compliance with the red blood cell infusion technique. As a result, the recipient's blood clotting is impaired; it begins to penetrate the walls of blood vessels, filling the cavities of the lungs and other parenchymal organs.
Symptomatically: the patient feels shortness of breath, the heart rate increases, pulmonary shock develops, and oxygen starvation develops. During the examination, the doctor cannot listen to the affected part of the organ; on an x-ray, the pathology looks like a dark spot.
Coagulopathy
Among all the complications that appear after blood transfusion, coagulopathy is not the least important. This condition is characterized by a coagulation disorder, resulting in massive blood loss syndrome with severe complications for the body.
The reason lies in the rapid increase in acute intravascular hemolysis, which occurs as a result of non-compliance with the rules for infusion of red blood cells or transfusion of different types of blood. With a volumetric infusion of red cells alone, the ratio of platelets responsible for coagulation is significantly reduced. As a result, the blood does not clot, and the walls of the blood vessels become thinner and more penetrating.
Kidney failure
One of the most severe complications after blood transfusion is acute renal failure syndrome, the clinical symptoms of which can be divided into three degrees: mild, moderate and severe.
The first signs indicating it are severe pain in the lumbar region, hyperthermia, and chills. Next, the patient begins
red urine is released, which indicates the presence of blood, then oliguria appears. Later, the state of “shock kidney” occurs; it is characterized by the complete absence of urine in the patient. In a biochemical study, such a patient will have a sharp increase in urea levels.
Anaphylactic shock
Anaphylactic shock is the most severe condition among allergic diseases. The cause of the appearance is the products included in the canned blood.
The first symptoms appear instantly, and immediately after the start of the infusion. Anaphylaxis is characterized by shortness of breath, suffocation, rapid pulse, drop in blood pressure, weakness, dizziness, myocardial infarction, and cardiac arrest. The condition never occurs with high blood pressure.
Along with pyrogenic and allergic reactions, shock is life-threatening for the patient. Failure to provide assistance in a timely manner can lead to death.
In an ocean of toxins
Zakiya Teregulova: Back in the 90s, the world's leading scientists warned about unprecedented pollution of the human internal environment, triggering a chain reaction of diseases, and the inability of the body to completely cleanse itself. This can be characterized as an endoecological crisis. Moreover, the accumulation of harmful substances in the human body is observed in the pericellular space that is difficult to access for purification.
— In what ways does intoxication of the body occur?
— 80-85% of toxins enter the body with food and water. According to official data, up to 60% of products, especially dairy products, are falsified and produced using substitutes and food additives, many of which are not just harmful, but dangerous: they are allergens, carcinogens, etc. Thus, unsaturated trans fats, which are widespread today, contribute to the development of atherosclerosis, diabetes mellitus, and accelerate the aging of the body. The ubiquitous PET container itself is, to a large extent, a pollutant of products.
A powerful toxic load haunts a person indoors: phenol-formaldehyde resins, which are used in the production of furniture, radiation from microwave ovens, cables, mobile phones, etc. Even bright children's toys - especially cheap Chinese ones - can cause intoxication, since the paint contains lead.
— How do environmental poisonings manifest themselves?
— But how can you cope, for example, with headaches or hypertension without medications?
— At the initial stage of hypertension, results can be achieved by cleansing blood vessels, optimizing nutrition and water balance. Headaches also do not occur by chance. To improve your health, you need, first of all, good nutrition and high-quality safe water.
— Are there effective cleansing methods?
To detoxify the body, you need to drink 35 ml of water per kg of weight in the cold season, 40-50 ml in the summer. The bathhouse has an unsurpassed lymphatic drainage and cleansing effect - many toxic substances are released through the sweat glands and skin. An effective method is walking with a light load. An excellent means of purifying the blood and normalizing lymph flow is hirudotherapy.
Transfusion of incompatible blood
The most dangerous consequences for the patient’s life are the consequences of transfused blood of different types. The first signs indicating the onset of a reaction are weakness, dizziness, increased temperature, decreased blood pressure, shortness of breath, rapid heartbeat, and lower back pain.
In the future, the patient may develop myocardial infarction, renal and respiratory failure, hemorrhagic syndrome with subsequent massive bleeding. All these conditions require immediate response from medical staff and assistance. Otherwise, the patient may die.
About children
Children are more difficult to tolerate various types and forms of intoxication. These phenomena are much more dangerous for them than for adults. In most cases, poisoning in children occurs stronger and faster than in adults, although the manifestations are practically no different. Only their appearance occurs a little earlier and they are more clearly expressed.
If a child has been poisoned, you should not hesitate to go to the hospital. It is necessary to make a correct diagnosis and prescribe effective treatment as soon as possible. This will help decide the fate of the baby.
Treatment of post-transfusion complications
After the first signs of post-transfusion complications appear, it is necessary to stop blood transfusion. Medical care and treatment are individual for each pathology, it all depends on which organs and systems are involved. Blood transfusion, anaphylactic shock, acute respiratory and renal failure require hospitalization of the patient in the intensive care unit.
For various allergic reactions, antihistamines are used for treatment, in particular:
- Suprastin;
- Tavegil;
- Diphenhydramine.
Calcium chloride solution, glucose with insulin, sodium chloride - these drugs are the first aid for potassium and citrate intoxication.
As for cardiovascular drugs, Strofanthin, Korglykon, Norepinephrine, Furosemide are used. In case of renal failure, an emergency hemodialysis session is performed.
Impaired respiratory function requires provision of oxygen supply, administration of euphilin, and in severe cases, connection to a ventilator.
a brief description of
So what is intoxication? This is poisoning of the body with various toxic substances that provoke disturbances in its functioning. Substances can enter the body from outside or form inside it.
Intoxication can manifest itself in quite a variety of ways. Symptoms depend on the toxic substance. Their accumulation in the body plays an important role. It is very important whether they arrived one-time or penetrate constantly, slowly accumulating. The concentration of a toxic substance in the body is also important.