Tuberculosis is a serious infectious disease with a high degree of contagiousness due to the ability to spread by airborne droplets. If there are disorders in the immune system, people from completely different social groups can get sick. Tuberculosis is not always a reflection of an antisocial lifestyle. It has several development options, one of them is tuberculosis intoxication (a manifestation of the childhood course of the disease).
Pulmonary tuberculosis is dealt with by specialists in the field of pulmonology using specific diagnostic methods.
Tuberculosis intoxication clinic
In tuberculosis intoxication, intoxication syndrome is the predominant (sometimes the only) clinical sign of the disease. Symptoms of local specific inflammation are not found in patients with tuberculosis intoxication. They often experience local nonspecific (paraspecific) changes caused by the presence of Mycobacterium tuberculosis in the body. These changes are most pronounced in the peripheral lymph nodes. Upon palpation, you can detect lymph nodes of five to nine groups enlarged to 5-14 mm in diameter, incl. supraclavicular and cubital. Lymph nodes are painless, mobile, soft-elastic consistency without signs of periadenitis and inflammation of the skin. Micropolyadenopathy is more pronounced in preschool children and to a lesser extent in adolescents and young adults. Hyperplasia of lymphoid tissue can also manifest itself as an enlargement of the liver and spleen.
In the chronic course of tuberculosis intoxication, the lymph nodes gradually decrease and become denser (sometimes to a rocky density).
TUBERCULOSIS INFECTION OF THE PRIMARY PERIOD
Advances in immunology of a theoretical and methodological nature have allowed researchers to sufficiently fully characterize systemic and local changes in immunological reactivity during the tuberculosis process. Primary infection with tuberculosis causes an immunological restructuring - the body becomes sensitive to tuberculin, and a tuberculin allergy develops. It is now recognized that delayed-type hypersensitivity, the main component of cellular immunity, is a leading factor in the immune mechanisms in tuberculosis.
The clinical period of primary tuberculosis infection takes 6-12 months from the moment of infection with tuberculosis, at this time the risk of developing the disease is highest. There is usually an asymptomatic preallergic period - the time from the penetration of Mycobacterium tuberculosis into the child’s body until the appearance of a positive tuberculin reaction, which averages 6-8 weeks, as well as a “turn” of tuberculin reactions - the transition of a negative reaction to a positive one. Essential for understanding tuberculosis is the uniqueness of immunobiological changes, which are characterized by the development, against the background of high sensitivity to tuberculin, of nonspecific allergic inflammatory processes in various organs and systems with a weakening of cellular immunity.
The early period of primary tuberculosis infection represents the initial phase of interaction between the tuberculosis pathogen and the macroorganism. During this period, MBT quickly spread by lymph and hematogenous routes throughout the body (latent microbiism), causing specific sensitization and paraspecific tissue changes. Paraspecific reactions disrupt the function of various organs, cause a variety of clinical symptoms, often causing diagnostic difficulties (“tuberculosis masks”). Currently, the early period of primary tuberculosis infection is almost asymptomatic in most children.
Systematic staging of RM with 2 TE allows detection of the early period of primary tuberculosis infection. A change in sensitivity to tuberculin due to recent MBT infection is called a “turn” of tuberculin reactions. When a “turn” is established, the child is sent to a TB specialist, who observes him for a year. After an early period of primary tuberculosis infection, the child remains infected with MTB (in the absence of risk factors for tuberculosis, subject to timely chemoprophylaxis), or local tuberculosis develops at different times after the primary infection (depending on the massiveness and virulence of the MBT, and on the state of the macroorganism). An intermediate form of the tuberculosis process before the development of the local tuberculosis process is tuberculosis intoxication. Subsequently, primary or secondary forms of tuberculosis develop.
TUBERCULOSIS INTOXICATION IN CHILDREN AND ADOLESCENTS
Tuberculosis intoxication in children and adolescents occurs when they become infected with tuberculosis and develop a primary tuberculosis infection without local manifestations determined by x-ray and other research methods. Tuberculosis intoxication is detected in children (adolescents) with first positive, increasing during observation and hyperergic reactions to tuberculin. It is characterized by the activity of the tuberculosis process and is accompanied by a deterioration in the general condition of the child (adolescent), which is expressed in the following:
- periodic increase in body temperature to subfebrile levels;
- loss of appetite;
- the appearance of neurovegetative disorders (increased nervous excitability or its depression, headache, tachycardia);
- slight enlargement of peripheral lymph nodes (micropolyadenia) with symptoms of periadenitis;
- slight enlargement of the liver, less often the spleen;
- stopping physiological gain or lack of body weight;
- tendency to intercurrent diseases;
- changes in the peripheral blood picture (mildly expressed acceleration of ESR, shift of the neutrophil count to the left, esinophilia, lymphopenia);
- change in immunological status (decrease in the number of lymphocytes and their functional activity).
The specificity of the described functional disorders must be confirmed by a thorough examination of the child (adolescent) to exclude nonspecific diseases. During the examination, it is necessary to use modern diagnostic methods, including direct and lateral radiographs, tomograms of the mediastinum in various projections, bronchoscopy, tuberculin provocation tests (hemotuberculin, immunotuberculin, etc.) before and after subcutaneous injection of tuberculin - 10-20 TU PPD-L, as well as bacteriological study.
Diagnosis includes a mandatory examination to exclude rare localizations of tuberculosis affecting the abdominal organs or small forms of tuberculosis of the intrathoracic lymph nodes.
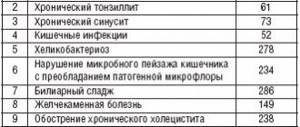
Differential diagnosis is carried out with chronic nonspecific lesions of the ENT organs, helminthic infestations and other diseases accompanied by signs of general intoxication syndrome.
Diagnostics
Timely diagnosis of the disease is extremely important for successful treatment. Often the diagnosis of tuberculosis is made to a child after all possible other diseases have been excluded, since there are no symptoms typical for tuberculosis. Often, diagnosis consists of a series of clinical studies, tuberculin testing, X-ray diagnostics, and bacteriological examination.
In a clinical blood test, leukocytosis, eosinophilia, lymphopenia and accelerated ESR are observed. These manifestations indicate intoxication.
A positive Mantoux test reaction is characteristic. On X-rays at the onset of the disease there are no signs of the disease, and they are also not detected in the extrapulmonary form of tuberculosis. But if a young patient has chronic intoxication due to pulmonary tuberculosis, an X-ray of the lungs will reveal an increase in the pulmonary pattern, emphysema and pleurisy are possible, small lesions are often identified: cavities, calcifications. Bacteriological diagnostics allows you to isolate the causative agent of the disease from the lesion and select the necessary antibiotic therapy.
Mantoux test
Modern laboratory diagnostics make it possible to avoid the Mantoux test and determine the disease with almost 100% probability. To do this, it is enough to take blood from the child for testing. Quite often, the quantiferon test is used, which consists of detecting specific interferon in the blood.
It is also quite common to use Diaskintest instead of the Mantoux test. It is more specific and more accurately determines the presence of mycobacteria than the tuberculin test. The technique of use is similar to Mantoux; inactivated bacterial particles are injected into the forearm and a reaction is expected. The disadvantage of these methods is their fairly high cost.
See also:
What is active and inactive tuberculosis and its symptoms
Treatment of tuberculosis intoxication
The most important thing in the treatment of tuberculosis intoxication is treatment with 2 anti-tuberculosis drugs: isoniazid 10-12 mg/kg or ftivazid 30 mg/kg in combination with ethambutol 20-25 mg/kg or prothionamide 20 mg/kg. If necessary, other drugs can be used. Treatment of early tuberculosis intoxication syndrome is carried out for at least six months.
In the treatment of tuberculosis intoxication in children and adolescents, general restorative methods are essential: adequate hygienic and dietary regimens, prolonged exposure to fresh air, and the gradual inclusion of tonic and hardening procedures. Great importance is attached to desensitizing therapy and vitamin therapy. In cases of severe retardation in physical development, anabolic hormones are indicated with correction of protein in the diet. Great importance should be attached to the identification and treatment of concomitant nonspecific diseases.
Dispensary observation - in group I for at least 6 months. During observation in group I, children and adolescents cannot attend children's and adolescent groups.
Subsequently, transfer to III B group, where they are observed for 2-3 years before deregistration.
Currently, children and adolescents are rarely diagnosed with tuberculosis intoxication. Behind the syndrome of chronic tuberculosis intoxication lies local tuberculosis, most often a minor form. Diagnostic capabilities today make it possible to find the cause of chronic tuberculosis intoxication syndrome and establish organ damage. Currently, the predominant diagnosis in children is tuberculosis of the intrathoracic lymph nodes.
When is medical help needed?
The above symptoms are a reason to contact a children's clinic, where the doctor will conduct the necessary examination. This:
- interviewing parents about the child’s possible contact with a patient with tuberculosis;
- palpation of lymph nodes;
- general blood analysis;
- exclusion of non-tuberculosis intoxication.
Careful inspection required
The presence of infectious diseases can produce symptoms similar to tuberculosis intoxication. To exclude this option, additional diagnostic methods are used.
Tuberculosis VGLU
The most common clinical form of primary tuberculosis, affecting various groups of VGLU. Inflammation most often develops in the lymph nodes of the bronchopulmonary and tracheobronchial groups, usually without involving lung tissue in a specific process. Tuberculous lesions of the lymph nodes of the bronchopulmonary group are often called bronchoadenitis.
After infection with Mycobacterium tuberculosis, a hyperplastic reaction develops in the lymph nodes, followed by the formation of tuberculous granulomas. The progression of specific inflammation leads to the gradual replacement of lymphoid tissue with tuberculous granulations. The area of caseous necrosis can increase significantly over time and spread to almost the entire lymph node. Paraspecific and nonspecific inflammatory changes occur in the tissue adjacent to the lymph node, bronchi, vessels, nerve trunks, and mediastinal pleura. The pathological process progresses and invades other, previously unchanged mediastinal lymph nodes. The total volume of local damage can be quite significant.
Depending on the size of the affected VLN and the nature of the inflammatory process, infiltrative and tumorous (tumor-like) forms of the disease are conventionally distinguished. The infiltrative form is understood as a predominantly hyperplastic reaction of the lymph node tissue with minor caseous necrosis and perifocal infiltration. The tumorous form is associated with pronounced caseous necrosis in the lymph node and a very weak infiltrative reaction in the surrounding tissues.
The course of uncomplicated VGLU tuberculosis is often favorable, especially with early diagnosis and timely treatment. Perifocal infiltration resolves, calcifications form in place of caseous masses, the lymph node capsule hyalinizes, and fibrous changes develop. Clinical cure with the formation of characteristic residual changes occurs on average 2-3 years from the onset of the disease.
Complicated or progressive course of VHL tuberculosis can lead to specific damage to the lung tissue. Lymphohematogenous and bronchogenic generalization of the process is observed in patients with progressive disorders in the immune system, which deepen against the background of tuberculosis. More often this occurs with late detection of the disease and inadequate treatment.
Video: tuberculosis and vaccination from Dr. Komarovsky
Read more:
Is computed tomography (CT) scanning harmful to human health?
How often can x-rays be taken without harm?
Is vaping harmful to health or not?✅
Is fluorography harmful ⛔ - how often can it be done for a child and an adult?
How harmful are headphones to a person's hearing and brain?
Article rating:
( 1 ratings, average: 5.00 out of 5)
Share with friends:
You may also be interested in:
Can children and adults eat crackers if they are poisoned?
Stages of acute and chronic poisoning in adults and children - symptoms and consequences
Causes of fainting during poisoning
Chronic endogenous intoxication of the body - syndrome, symptoms and treatment
Clinic
The severity of symptoms caused by damage to the respiratory organs depends on the prevalence of the process and the caseous-necrotic component of specific inflammation, as well as the phase of the inflammatory reaction. In infants and young children, local forms of primary tuberculosis are characterized by striking clinical manifestations. At older ages, their symptoms are often quite sparse.
In small forms of VGLU tuberculosis, no more than 2 VGLUs are affected by specific inflammation, and their diameter does not exceed 1.5 cm. Minor forms of VGLU tuberculosis often occur without obvious clinical manifestations. The disease is diagnosed mainly by the variation of sensitivity to tuberculin and X-ray data, mainly CT.
VGLU tuberculosis with a large volume of lesions usually begins subacutely, with a gradual increase in symptoms of intoxication. With a pronounced exudative perinodular reaction involving all groups of lymph nodes of the root of the lung and mediastinum in the pathological process, the disease develops acutely. In this case, febrile fever and general functional disorders are noted. Patients may develop a characteristic dry whooping cough (whooping cough). In some patients, the pressure of enlarged lymph nodes on the bifurcation of the trachea and the mouth of the main bronchi causes the appearance of stridor breathing.
Narrowing of the lumen of the superior vena cava by enlarged lymph nodes of the mediastinum leads to a more or less pronounced syndrome of the superior vena cava: on the anterior surface of the chest on one or both sides the network of saphenous veins expands. When the superior vena cava is compressed, other symptoms are sometimes expressed: headache, cyanosis and puffiness of the face, increased volume of the neck, increased venous pressure.
Stetoacoustic symptoms of tuberculous lesions of the upper lymph nodes are caused by perifocal nonspecific inflammatory changes in the mediastinum. A muffled percussion sound is detected in the parasternal and paravertebral zones, increased bronchophony over the spinous processes of the thoracic vertebrae, and a venous spinning noise over the upper part of the manubrium of the sternum when the head is sharply thrown back. Without a perifocal inflammatory reaction, it is impossible to detect an increase in VLN using physical methods.
Prevention
The main method of preventing tuberculosis intoxication is BCG vaccination, which forms the resistance of immunity to the tuberculosis bacillus. This, unfortunately, does not mean that the child will be 100% protected from infection, but in vaccinated children, tuberculosis microbacteria do not enter the blood, but remain in the lymphatic fluid.
If, nevertheless, the disease cannot be avoided, then it will proceed easier and with minimal consequences. Therefore, you should not refuse Mantoux tests carried out in schools, which help prevent the possible risk of developing severe pathology, because the price of the child’s life is at stake.
One of the methods of preventive control is the Mantoux test.
If your child has symptoms of tuberculosis intoxication, you should not wait until they go away on their own. At the first suspicion of infection, you should consult a doctor. The video presented in this article will allow our readers to find out what to do when symptoms of tuberculosis intoxication appear.
general information
Most often, tuberculosis intoxication is detected in children and adolescents. However, in mature and elderly patients, a pathological process is also possible, manifested in the form of tuberculosis intoxication.
Endogenous poisoning by waste products of bacilli is detected during the first year after infection. The fact of infection of the body with Mycobacterium tuberculosis confirms the change in the tuberculin test (a change in its result from negative to positive), which is evidence of the formation of specific protective reactions.
The duration of tuberculosis intoxication as a variant of primary tuberculosis in most cases does not exceed 8 months . This form of tuberculosis most often has a favorable prognosis. Inflammatory tissue damage gradually fades away. The resulting single tuberculous granulomas (nodules with a high level of metabolism) are replaced by connective tissue with the formation of a scar or petrification (an area encrusted with calcium salts).
Reference materials (download)
| # | File | file size |
| 1 | Article. Chronic tobacco intoxication as a factor in reducing the concentration of antibiotics in the treatment of pulmonary tuberculosis and CP.2019 | 235 KB |
| 2 | Detection and diagnosis of tuberculosis in children entering and studying in educational institutions. Clinical recommendations. 2017 | 817 KB |
| 3 | Multidrug-resistant respiratory tuberculosis in children. Clinical protocols of the Ministry of Health of the Republic of Kazakhstan - 2018 | 1 MB |
| 4 | Federal clinical guidelines for the diagnosis and treatment of latent tuberculosis infection in children. ROF.2015 | 374 KB |
| 5 | Article. Features wedge. course and chemotherapy of tuberculosis in children from foci with a different spectrum of drugs. sensitive.2019 | 778 KB |
| 6 | Disease history. Primary tuberculosis complex, infiltration phase. Pediatrics | 43 KB |
| 7 | Disease history. VDT (20.11.2010) intrathoracic lymph nodes (root), tumorous form, infiltration phase. Pediatrics | 97 KB |
| 8 | Disease history. VDTB (02/07/2014) of unknown location; Destr -; MBT - (M -, K -), resist 0; Gist 0; Cat 3; Cog 1 (2014) Pediatrics | 200 KB |
Symptoms
The disease is characterized by a nonspecific clinical picture and the absence of pronounced foci of infection in the organs. The picture of tuberculosis intoxication is characterized by general symptoms of infection and signs of an allergic reaction. There are no symptoms such as cough, shortness of breath, hemoptysis or chest pain.
Early intoxication
Early tuberculosis intoxication is the initial period of the disease, developing against the background of fresh (primary) infection with mycobacteria. The following symptoms are possible:
- Irritability.
- Constant headache.
- Sleep disorders (frequent awakenings at night, restless sleep, difficulty falling asleep).
- Low-grade fever (does not exceed 38ºC).
- Night sweats.
- Poor appetite.
- Rapid fatigue during mental and physical work.
- Decline in school performance.
- Lymphadenopathy (enlarged peripheral lymph nodes). Become a soft-elastic consistency. Most often, several groups of lymph nodes are affected at once (axillary, cervical, inguinal).
- Dyspepsia. Children may have bowel movements (constipation or diarrhea) and pain in the epigastric or periumbilical area.
- Enlarged liver and spleen. It is more often observed in people of thin build.
- Erythema nodosum. Dense nodes up to 4-5 cm in size form on the body (most often on the lower extremities). They are located deep under the skin. There is pain and soreness. There is no skin itching. After a few days, they resolve with the formation of areas of tissue compaction. The onset of erythema nodosum is accompanied by fever, chills, joint pain and general malaise.
The first stage of intoxication lasts about 4-6 weeks. Upon completion, a tuberculin test occurs (a positive reaction to tuberculin administration is detected for the first time).
Chronic intoxication
Signs of chronic tuberculosis intoxication are:
- Constant fatigue that does not disappear with long rest.
- Psycho-emotional disorders (irritability, tearfulness, mood instability).
- Autonomic disorders (pressure changes, unstable stools, rapid heartbeat, sweating).
- Sleep disturbance.
- Cardiovascular disorders (tendency to lower blood pressure, heart murmur).
- Loss of body weight.
- Enlargement of 6-9 groups of lymph nodes at once.
- Frequent inflammatory eye diseases (inflammation of the conjunctiva and cornea).
- Dyspepsia.
- Children's retardation in physical development.
- Periodic moderate rise in temperature.
Symptoms of the patient's condition
Early tuberculosis intoxication is expressed in an imbalance of the nervous system. After this, other body systems begin to suffer. Most often, at the very beginning of poisoning, the child exhibits inexplicable changes in behavior. Changes are expressed in:
increased irritability; high excitability; worsening attention problems; headaches; sleep problems
The patient experiences a decrease in appetite, as well as pale skin. Dullness of the skin is often accompanied by a low-grade fever. Additional symptoms include enlargement of the liver and spleen. In guys with a thin build, such drastic changes are visible even with the naked eye.
Much less often, young patients complain of any significant problems with the digestive system. There are isolated cases of significant weakening of the intestines, as well as regular constipation.
One of the most important alarm bells for parents should be a sudden stop in weight gain. Such a failure or a sudden lack of body weight is not typical for a growing body. To monitor suspicions, you need to take regular measurements of the child's weight every month at a young age. Schoolchildren are usually weighed no more than once a year.
A few more points should be an important aspect for emerging suspicions:
- Loss of body weight is not always observed among infected children. You should not rely only on this point, relaxing after the control weighing did not show negative results.
- Patients often suffer from bronchoadenitis. This indicates significant changes in the size of individual lymph nodes located in the bronchi. An x-ray taken during this period will show signs of extensive inflammation in the indicated area.
- Mycobacterial components are distributed through the bloodstream to different organs.
Doctors always warn parents and guardians that a child after pathology is prone to various complications of varying degrees of severity. Most often they are expressed in the form of tuberculous meningitis.
Reasons for development
Early tuberculosis intoxication means the appearance of tuberculosis with the impossibility of establishing the exact localization of inflammation. This occurs when the body is susceptible to a given disease. Moreover, with the help of an examination, the presence of mycobacteria and their reproduction is confirmed, but the place of development of this process cannot be determined. This type of tuberculosis is typical for children, but for adults there is a different condition. Tuberculosis intoxication in adults occurs as poisoning as a result of an advanced form of the disease.
Tuberculosis intoxication is the primary form of the disease, which occurs in 12% of all cases of tuberculosis. This diagnosis is made when the child has stable positive indicators of the Mantoux injection.
These pathogenic microorganisms enter the body through the respiratory system, after which macrophages begin to fight them, which transfer them to the lymphatic system, where they live quietly for some time. Having waited for the most convenient time, when immunity decreases, mycobacteria begin to multiply intensively.
The main cause of tuberculosis intoxication is the direct contact of children with mycobacterium tuberculosis, which can enter the child’s body using the following methods:
- Alimentary – characterized by infection through food products, most often meat and milk;
- Aerogenic – is the leading method of infection, it consists of airborne transmission;
- Contact-household – occurs quite rarely, in 5% of all cases of disease;
- Transplacental - based on infection through the placenta from a sick mother.
Of course, this disease can occur in any child, but there are children who are at risk and have a predisposition to this pathology. Most often these are children:
- those who have not been vaccinated with BCG;
- in contact with a sick person or animal;
- having a persistently positive Mantoux test;
- having a genetic predisposition;
- patients with HIV infection or AIDS;
- overloaded with stressful situations;
- having a history of chronic diseases;
- taking hormonal drugs for a long time;
- from socially disadvantaged families;
- arrived from Asian countries;
- dramatically changed climatic conditions.
Pathogenesis
Massive production of toxins occurs during the circulation of bacteria in the circulatory system before the formation of a focus of infection. After some time, toxemia develops - poisoning of the body caused by the presence of toxins in the blood. This phenomenon enhances the specific sensitivity of tissues to foreign substances - Koch's bacilli and their metabolic products. A number of pronounced toxic-allergic reactions of tissues develop.
During the period of tuberculosis intoxication, colonies of Mycobacterium tuberculosis are concentrated in the structures of the lymphatic system. The bacilli gradually settle in biological filters - lymph nodes, initiating their hyperplasia (enlargement, proliferation). The result of this process is micropolyadenopathy - the appearance of a chain of small, dense, painless lymphoid nodules.