Opiate poisoning (methadone, heroin, morphine) - an overdose, develops in people who have taken a dose that is excessive for their body. The pathology occurs most often in drug addicts. Against the background of the presence of poisons in the blood and organs of the patient, a typical clinical picture is revealed. The most characteristic manifestations of this condition are: cyanotic coloration of the skin, sharply constricted pupil and loss of consciousness. The amount of a psychoactive substance (surfactant) that leads to acute intoxication when it enters the body is different for each individual. The degree of toxic damage depends on personal characteristics, health status, and the stage of addiction to the drug.
The effect of opiate drugs on the body
Basically, opiate drugs have an analgesic effect, that is, pain relief. Due to the peculiarities of the chemical structure and physical properties, these drugs are conventionally divided into narcotic and non-narcotic. The former have a pronounced effect, strong pain relief, but contribute to addiction and cause drug cravings. The latter have a relatively weak result, but are safer for use.
Regardless of the group, any opiate analgesic always provokes the risk of addiction, since opiates do not promote wound healing or neutralize pain triggers in the body, but directly affect the central nervous system. Penetrating into cells, they change the very perception of pain and cause euphoria. In other words, opiates simply cause a certain intoxication and, for some time, break the worldview laid down by nature.
Structure of opioids
The chemical structure of opioids is very diverse. Their most common component is a benzene ring, which is connected by a propyl or ethyl “bridge” to a nitrogen atom. This is what ensures the similarity of opioids to tyrosine, an amino acid that is part of enkephalin (the simplest opioid peptide) and plays an important role in its interaction with opioid receptors.
The nitrogen atom is most often represented here as a component of the piperidine ring. A large proportion of opioids are tertiary amines.
Causes of opiate poisoning
Opiates primarily affect a person's sensations through opioid receptors (a type of nerve ending in the central brain). When exposed to these substances, neurons reduce their sensitivity, thus helping to tolerate painful feelings. When drugs enter the brain excessively, the functions of the nervous system begin to malfunction, causing negative changes in the body’s condition and opiate poisoning.
The cause of poisoning with this type of drug can only be an overdose. It can take the form of intentional (criminal, suicidal, narcotic) and unintentional (accidental, careless). The criminal form involves attempts on the life of another person through the secret or open introduction of opioid substances to him. Suicidal and narcotic means the use of analgesics with the aim of committing suicide or obtaining drug intoxication. The unintentional form means a tragic coincidence of circumstances in which the concentration of the drug taken exceeded the norm. This event often happens to young children left unattended, or the cause is an incorrect prescription of antitussives.
Treatment with opiates is possible only after a doctor’s prescription and only under his close supervision. A dose of 0.5-1.5 mcg/kg can be considered safe for the human body. If the amount of one dose is incorrectly calculated, the first serious symptoms appear, predicting poisoning. If an increased dose is used regularly, then significant disruption of the functioning of many organs and systems can occur. It is worth noting that an overdose of opiates in the worst cases can also be fatal.
Excessive amounts of medication cannot be eliminated by the body on its own or remain in the body without consequences. Therefore, all human organs signal danger. Severe symptoms help avoid serious consequences.
Gradation of opioids by structure
What drugs are considered opioids under this classification? Containing the following elements:
- Phenanthrenes (4,5α-epoxymorphinans) are natural or semi-synthetic opioids, similar in structure to morphine, i.e., having a piperidine and an aromatic ring. These are heroin, codeine, morphine, hydrocone, oxycodone, naloxone, 6-monoacetylmorphine, buprenorphine, nalbuphine, oxymorphone.
- Morphinans. Their structure differs from the structure of morphine by the epoxy “bridge” removed. They are also distinguished by their purely synthetic origin. These are dextromethorphan, levorphanol, butorphanol.
- Benzomorphans are compounds such as phenazocine, metazocine, and pentazocine.
- Diphenylheptanones.
- Phenylpiperidines.
- 4-anildopiperidines.
Symptoms of acute poisoning
In case of opiate poisoning, the symptoms are pronounced. First of all, the effect of a “pinpoint” pupil is noticeable. Its size is reduced to a minimum, visually the pupil looks like a poppy seed, which has an extremely unnatural appearance. In parallel with this, the second sign of the triad is accompanied by difficulty breathing. When opioids act on β-receptors, ventilation of the lungs worsens, breathing rate and the volume of inhaled air are disrupted.
The first two signs of opiate poisoning carry some danger, but the most terrible is the third most important sign of the triad of symptoms of opiate poisoning. The risk is due to the likelihood of coma. At first, the victim has a depressed state, foggy consciousness, and drowsiness. The functioning of the organs of vision and hearing is disrupted, and a certain stupor occurs. In exceptional cases, for example, after heroin poisoning, the patient enters a phase of euphoric happiness, the mood becomes elevated.
Morphine behaves in the opposite way; due to its ability to penetrate the blood-brain barrier, poisoning with this substance does not cause joyful sensations. Only analgesic and sedative effects are expressed in this case. Poisoning with codeine and dextromethorphan also has some specifics. An overdose of these medications provokes an antitussive effect.
Main types of cancer pain
Morphine and other opioids are the mainstay of pain treatment in cancer patients. In 1986, WHO proposed a simple three-step model for cancer pain relief (Figure 2a). The WHO emphasizes that “alleviating psychological, social and spiritual problems is of paramount importance” [1].
Rice. 1 | WHO principles for the use of analgesics for pain relief in cancer are: a) according to pain level b) orally c) hourly d) individualized approach and e) attention to detail. (WHO 1986)
Acute cancer pain
- Tumor-associated: pathological fracture, obstruction or perforation of a hollow organ, perforation of the superior vena cava.
- Associated with antitumor therapy: mucositis, headache, hand-foot syndrome, myalgia and arthralgia.
- Associated with radiotherapy: mucositis, bone pain, neuropathy.
- Acute postoperative pain.
Chronic cancer pain
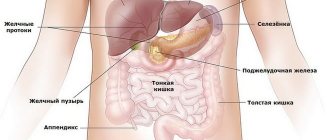
- Associated with a tumor: - bone pain - metastases, infiltration into the bone marrow; - pain in soft tissues - headache, facial pain, pleural pain; - visceral pain - liver enlargement, chronic intestinal obstruction, pain in the perineum.
- Cranial neuralgia: glossopharyngeal neuralgia, trigeminal neuralgia.
- Plexopathies: brachial, lumbosacral and cervical.
- Radiculopathies: lumbosacral, cervical and thoracic.
- Neuropathy: paraneoplastic sensory neuropathy.
- Pain associated with chemotherapy: avascular necrosis, vertebral compression fractures, peripheral neuropathy.
- Surgical pain: lymphedema, post-thoracotomy pain, phantom amputation pain, post-mastectomy pain.
- Pain associated with radiotherapy: cystitis, enteritis or proctitis, osteoradionecrosis and fractures; painful secondary malignant neoplasms, brachial and lumbosacral plexopathies.
- Pain associated with hormonal therapy: arthralgia, myalgia, dyspareunia, gynecomastia, osteoporotic compression fractures.
Opioids bind to opioid receptors in the nociceptive pathway to reduce impulse transmission and pain perception in the somatosensory cortex. Opioid medications include morphine, oxycodone, hydrocodone, tramadol, hydromorphone, oxymorphone, fentanyl, buprenorphine, and methadone [2].
Morphine. It is considered the number one drug for cancer-related pain, mainly because it is relatively more common and available, but no more effective than other opioids [3].
Methadone. The use and titration of methadone is complex and should be carried out by professionals with a high level of expertise, such as specialists in palliative care and pain management [3].
Buprenorphine. Concerns have been raised about the effectiveness of buprenorphine due to its partial agonist activity, which may result in decreased analgesic effect and increase the likelihood of side effects at higher doses. Some studies have shown this drug to be safe and effective in the treatment of chronic cancer-related pain [4] and have suggested it as an alternative to morphine, oxycodone, and fentanyl [5]. Parenteral buprenorphine formulations and low-dose transdermal buprenorphine formulations are approved for the treatment of moderate to severe chronic cancer pain [6].
Patients need access to both sustained-release opioids and immediate-release medications to manage episodes of acute, severe pain. Extended-release tablets are usually the drug of choice due to the ability to provide patients with lower dosages, longer-lasting analgesic effects, and less impact on sleep than immediate-release tablets, but their cost may limit patients' ability to purchase them [3].
Also, opioids with different rates of release of the active substance have different side effects. Immediate-release drugs have a stronger effect on the limbic system and produce euphoria more quickly than extended-release drugs. Long-acting opioid analgesics may be considered for the treatment of patients with chronic cancer pain, including a history of non-medical opioid use [2].
The transdermal route of drug administration (fentanyl, buprenorphine) is used in patients who are unable to take medications orally. The subcutaneous route is used in patients who cannot receive opioids via the oral or transdermal route. The intravenous route of administration should be considered when opioid titration is necessary or for rapid pain relief. Rectal administration of opioids can also be effective, but is limited by the availability of appropriate drugs and patient desire [3].
Inhaled and intravenous opioids enter the bloodstream and cross the blood-brain barrier more quickly. Inhaled and intravenous drug use has been shown to be associated with an increased risk of substance use disorders and overdose [11].
Dose
Clinicians should select the minimum effective dose of opioid that will produce the desired analgesia with little or no side effects. Numerous studies have shown that high-dose opioid prescriptions (usually >100 mg per day) are associated with an increased risk of abuse [12] and/or overdose in patients with both chronic cancer pain and other types of chronic pain syndromes [13]. The US Centers for Disease Control and Prevention guidelines for the treatment of non-cancer pain state that clinicians should avoid dosages > 90 mg per day [9]. However, dose and time limits are not always appropriate for patients with chronic cancer pain, who often require increased doses over long periods of time [2].
Side effects of opioids include constipation, nausea and vomiting, pruritus, sedation, opioid neurotoxicity, and respiratory depression. Opioid-related side effects can be controlled by reducing the dose, using a different opioid, changing the route of administration, or symptomatic management of the side effects. Concomitant use of antihistamines, anxiolytics, or gabapentinoids to treat symptoms associated with pain may increase opioid toxicity [2].
Adjuvant analgesics, including anticonvulsants such as amitriptyline and gabapentin, are considered particularly effective for neuropathic pain, but must be carefully selected to prevent increased central nervous system side effects when used concomitantly with opioids. Gabapentin should be used with caution for neuropathic pain: additional studies are needed to evaluate the effectiveness and safety of this drug. NSAIDs and acetaminophen can be used as opioid-sparing agents for bone pain in the absence of contraindications [2].
Patients are at increased risk of opioid overdose early in the initiation of opioid therapy or later due to the development of opioid tolerance. Patients with episodes of non-medical opioid use and a history of substance use disorders are extremely vulnerable to overdose on these drugs after a period of abstinence: while the desire to use opioids persists, they lose the sensitivity to them that previously prevented sedation and respiratory depression . Loss of tolerance to opioids typically occurs within a few days of stopping the drug, while cravings associated with non-medical opioid use and substance use disorders can persist for months and years [10].
Most opioid prescribing guidelines [9,14,15] encourage optimized use of non-opioid and adjuvant analgesics [3,14,15].
Prescribing Naloxone
Naloxone is a short-acting opioid antagonist used as an antidote for opioid overdose, helping to reduce the risk of respiratory depression; may be useful for patients at risk for non-medical opioid use episodes [2].
Mechanism
Nociceptive information about peripheral tissue damage is transmitted through an afferent nerve fiber to the dorsal horn of the spinal cord, where it synapses with a second neuron and then allows the impulse to travel up the spinal cord. The second-order neuron then synapses with a third-order neuron in the thalamus, which finally sends information to the somatosensory cortex, resulting in the perception of pain intensity [7]. In addition to this main spinothalamic pathway, nociceptive input is also transmitted through other pathways, resulting in arousal and/or sleep disturbance, negative emotions associated with the presence of pain and treatment planning [8] (Fig. 2).
Rice. 2 | Major ascending nociceptive pathways
Four common neurological pathways are involved in the perception of pain and its associated effects. Tumor tissue and inflammation stimulate nociceptors in peripheral tissue, generating a nociceptive impulse. This impulse is then transmitted through afferent nerves to the dorsal horn of the spinal cord. The impulse usually follows a major pathway along the spinothalamic tract and projects to the somatosensory cortex, resulting in the perception of pain intensity and severity. The impulse can also be transmitted along the limbic system, which leads to negative emotions associated with the presence of pain. Transmission through the reticular activating system leads to agitation and sleep disturbance, and transmission through the prefrontal cortex leads to anxiety and preoccupation.
Expression of μ-opioid receptors is found throughout the nervous system, including the periphery, spinal cord, thalamus, somatosensory cortex, midbrain, and limbic system, and opioids bind to any μ-opioid receptor they detect. Stimulation of the μ-opioid receptor in the ventral tegmental area of the midbrain and nucleus accumbens in the ventral striatum results in the release of dopamine, opioid peptides and serotonin (Figure 3) [8].
Rice. 3 | Conceptual model of the effects of opioids on nociceptive and nonnociceptive pathways.
Opioids stimulate μ-opioid receptors (MORs) in the nociceptive pathway, resulting in a rapid decrease in nociceptive transmission in pain. Over time, the slow release of excitatory amino acids leads to the development of tolerance and hyperalgesia. Stimulation of the MOR in the limbic pathway results in the rapid release of neurotransmitters (including dopamine, opioid peptides, and serotonin) that produce feelings of euphoria and/or pleasure. Over time and due to the absence of opioids, pathways become active leading to the release of neurotransmitters such as corticotropin releasing factor, norepinephrine and dynorphin, causing dysphoria and/or distress
These neurotransmitters lead to euphoria and thereby reduce the negative effects of pain and other experiences associated with a cancer diagnosis, fear of death, loss and/or family, personal or financial problems. Patients with relatively higher concentrations of the μ-opioid receptor in their limbic system experience a particularly intense response to opioid administration [19]. This may lead them to non-medical use of opioids. Gradually, the release of neurotransmitters associated with pleasure after opioid use decreases, and the release of neurotransmitters in the amygdala associated with dysphoria and stress increases [8]. These neurotransmitters include corticotropin releasing factor, norepinephrine, dynorphin, and orexin. As a result, patients tend to increase their opioid doses due to the increasing accumulation of μ-opioid receptors in the limbic system. Over time, patients who eventually develop a substance use disorder will increase their opioid use not only to regain the euphoric effects, but also to prevent those dysphoric feelings and simply to restore a state of “normalcy” [2].
Substance use disorder is defined by 11 diagnostic criteria covering four main areas: features of control disorders, social impairment, risky use, and pharmacological criteria. Substance use disorder can be classified as mild (2–3 criteria), moderate (4–5 criteria), or severe (≥ 6 criteria) [16].
Behaviors associated with non-medical use of opioids (NMIO) [2]:
- frequent unscheduled doctor visits or phone calls asking for opioid prescriptions;
- requiring an excessively large dose of opioids that does not correspond to the severity of the patient's pain syndrome;
- reports of lost or stolen prescriptions;
- frequent visits to the emergency room to obtain opioids;
- patient search for opioids from multiple sources;
- requests for a specific opioid;
- resistance to changes in opioid regimen even when clinically indicated;
- use of unregulated restricted or illicit drugs;
- requiring opioids to be prescribed to achieve euphoria or to treat symptoms such as anxiety or insomnia;
- reports of problems in daily life due to opioid use;
- family members and/or caregivers express concerns about the patient's opioid use;
- drug supplies found on the patient;
- obtaining opioids from non-medical sources;
- reports of theft, falsification or forgery of opioid prescriptions;
- discrepancy between the number of medications taken and those prescribed, lack of explanation for this.
Current monitoring
Evidence-based recommendations for the safe prescribing of opioids in patients with cancer pain are limited [9,14,15]. The American Cancer Society has developed guidelines for the management of pain in cancer survivors [14], and the US National Comprehensive Cancer Network has issued guidelines for the management of cancer-related pain in adults [17]. Current evidence suggests a universal precautions approach consisting of initial screening of all patients with cancer pain who require opioids using risk assessment tools [2].
Patients at high risk for non-medical opioid use will require enhanced monitoring. Before initiating opioid use, physicians should educate patients about the potential risks, benefits, alternatives, and possible side effects associated with opioid therapy, as well as inform them about safe practices for the use, storage, and disposal of opioids [14]. Selection, initial dosage, and maintenance doses of opioids should be tailored to individual patient characteristics, such as pain intensity level and the presence of renal or hepatic dysfunction [15]. A clear plan for stopping opioid treatment should be discussed in advance with the patient if the etiology of pain suggests an expected time of cessation, such as treatment-related oral mucositis in patients undergoing stem cell transplant or radiation therapy for head and neck cancer [2].
Prescription drug monitoring programs
Prescription drug monitoring programs exist in North America, Australia and parts of Europe. These programs collect information about controlled substances filled by a pharmacy, analyze it in a secure electronic database, and make the data available to authorized users, including prescribers, regulators, and law enforcement agencies. Prescription drug monitoring programs show when and where patients received opioid prescriptions and who prescribed them, and can identify patients who seek opioids from multiple prescribers (“commercial shopping”) or fill multiple prescriptions at different locations. pharmacies (“purchase at a pharmacy”) [2].
Taking action
Measures that are commonly used to address non-medical opioid use include: clearly communicating the steps to be taken in the event of repeated non-adherence, reducing the time interval between subsequent refills to ensure more frequent and vigilant monitoring, limiting the amount of opioids and refill doses, opioid withdrawal when possible, referral to a pain, palliative care, mental health, or addiction specialist for co-management [15]. Education regarding the safe use, storage and disposal of opioids should be provided to both patients and their caregivers. The ultimate goal of opioid therapy in patients with episodes of non-medical opioid use is to achieve acceptable pain relief, improve physical and psychosocial function, and minimize complications to optimize the risk-benefit ratio to ensure safe opioid use [2].
Rice. 4 | General approach to the management of cancer patients on chronic opioid therapy.
a) Universal screening includes interviews and the use of risk assessment tools (CAGE - Risk Assessment Questionnaire, SOAPP - Screening for Opioid Need for Pain Patients, ORT - Opioid Risk Assessment Tool). b) Enhanced monitoring includes the use of prescription drug monitoring programs, random urine drug testing, and close behavioral monitoring to identify pathological signs associated with opioid use. c) Non-medical use of opioids (see Behaviors Associated with Non-Medical Use of Opioids) d) Additional strategies include reducing the time interval between follow-up studies for repeat prescriptions, limiting the amount of opioids and dosage of refills, setting limits, stopping opioids at the earliest opportunity, referral to a specialist for further management. NMIO - non-medical use of opioids.
Patients with advanced cancer develop a range of physical and psychological symptoms, and pain is often treated in the context of a variety of associated problems, such as fatigue, nausea, emotional distress, and delirium. More than half of people observed using non-medical opioids received prescription opioids from a friend or relative free of charge, and 11% purchased opioids from the same individuals [18]. Following the opioid overdose epidemic, calls have been made for clinicians to reconsider the practice of prescribing opioids to patients at the end of life. There are currently no regulations for the safe prescribing of opioids, but it may be worthwhile to ensure free legal access to opioids for certain people with terminal illnesses [2].
Literature:
- Dalal S., Bruera E. Access to opioid analgesics and pain relief for patients with cancer //Nature Reviews Clinical Oncology. – 2013. – T. 10. – No. 2. – P. 108.
- Arthur J., Bruera E. Balancing opioid analgesia with the risk of nonmedical opioid use in patients with cancer //Nature Reviews Clinical Oncology. – 2020. – P. 1.
- Caraceni A. et al. Use of opioid analgesics in the treatment of cancer pain: evidence-based recommendations from the EAPC //The lancet oncology. – 2012. – T. 13. – No. 2. – pp. e58-e68.
- Pergolizzi J. et al. Current knowledge of buprenorphine and its unique pharmacological profile //Pain Practice. – 2010. – T. 10. – No. 5. – pp. 428-450.
- Schmidt-Hansen M. et al. Buprenorphine for treating cancer pain // Cochrane Database of Systematic Reviews. – 2020. – No. 3.
- Foster B. et al. Buprenorphine // Journal of pain and symptom management. – 2013. – T. 45. – No. 5. – pp. 939-949.
- Renn CL, Dorsey SG The Physiology and Processing of Pain A Review //AACN Advanced Critical Care. – 2005. – T. 16. – No. 3. – pp. 277-290.
- Koob GF, Volkow ND Neurobiology of addiction: a neurocircuitry analysis //The Lancet Psychiatry. – 2020. – T. 3. – No. 8. – pp. 760-773.
- Dowell D., Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2020 //Jama. – 2016. – T. 315. – No. 15. – pp. 1624-1645.
- Volkow ND, McLellan AT Opioid abuse in chronic pain—misconceptions and mitigation strategies //New England Journal of Medicine. – 2020. – T. 374. – No. 13. – pp. 1253-1263.
- European Monitoring Center for Drugs and Drug Addiction (EMCDDA). Preventing opioid overdose deaths with take‐home naloxone. – 2020.
- Comer SD et al. Abuse liability of prescription opioids compared to heroin in morphine-maintained heroin abusers //Neuropsychopharmacology. – 2008. – T. 33. – No. 5. – P. 1179.
- Bohnert ASB et al. Association between opioid prescribing patterns and opioid overdose-related deaths //Jama. – 2011. – T. 305. – No. 13. – pp. 1315-1321.
- Paice JA et al. Management of chronic pain in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline //Journal of Clinical Oncology. – 2020. – T. 34. – No. 27. – pp. 3325-3345.
- Chou R. 2009 Clinical Guidelines from the American Pain Society and the American Academy of Pain Medicine on the use of chronic opioid therapy in chronic noncancer pain: what are the key messages for clinical practice? //Polskie Archiwum Medycyny Wewnetrznej. – 2009. – T. 119. – No. 7-8. – pp. 469-477.
- American Psychiatric Association et al. Diagnostic and statistical manual of mental disorders (DSM-5®). – American Psychiatric Pub, 2013.
- National Comprehensive Cancer Network et al. NCCN clinical practice guidelines in oncology–adult cancer pain (version 1.2018) //NCCN https://www. nccn. org/professionals/physician_gls/pdf/pain. pdf. – 2020.
- Lipari RN, Hughes A. How people obtain the prescription pain relievers they misuse //The CBHSQ report. – Substance Abuse and Mental Health Services Administration (US), 2020.
- Reed B. et al. Genetics of opiate addiction //Current psychiatry reports. – 2014. – T. 16. – No. 11. – P. 504.
First aid
First aid should be started immediately after symptoms are detected. Immediate help will increase the chances of recovery. All actions should be directed in the following main directions:
- Eliminate the possibility of further entry of opiates into the victim’s body.
- Urgent call for an ambulance.
- In case of oral intoxication (poisoning when taking drugs by mouth), it is necessary to urgently perform gastric lavage. The patient is given to drink as much water as possible (at least a liter) and reflex vomiting is induced. This procedure must be carried out at least 4–5 times. This will remove opiate substances that have not yet entered the blood from the body.
- If respiratory arrest or cardiac arrest occurs, resuscitation measures must be started immediately. In this case, it is necessary to perform artificial respiration and chest compressions before the ambulance arrives.
It is strictly forbidden to give coffee or alcoholic beverages to a person who is poisoned by opiates.
Any substances that have an effect on the central nervous system can aggravate the situation or even lead to death. If there is a possibility that the victim is HIV-infected, then when contacting him, it is imperative to take protective measures.
Gradation of opioids by origin
So, opioids. How do they relate to this group? Drugs divided into several smaller gradations:
- Natural, plant: opium poppy alkaloids: thebaine, morphine, codeine;
- other plant opioids: salvinorin A, mitragynine.
Therapeutic treatment, review of drugs
After first aid is provided, the victim should be treated by professionals. The first thing you need to do is administer an antidote to the patient. In this case, the antidote for opiate poisoning is naloxone hydrochloride. Its action is aimed at completely or partially eliminating symptoms. Naloxone is a pure opiate and opioid antagonist. The disadvantage of this remedy is that in conditions of depressed breathing its effectiveness is reduced to zero.
This antidote for opiate poisoning has a short-term effect. It lasts about 45 minutes. In the case of intramuscular administration, the effect lasts slightly longer. Therefore, you need to pay maximum attention to the patient. At any moment, all the negative symptoms of poisoning can reappear.
During treatment, symptomatic therapy is carried out. It includes measures to restore breathing, namely the organization of artificial respiration of the patient with an Ambu bag, intubation of the trachea, after which the victim is connected to an artificial respiration apparatus.
During hospitalization, the following drugs are used:
- Mexidol (has a positive effect on the central nervous system);
- theomide bromide (normalizes nervous excitation in synapses);
- glucose (maintains the general condition of the body);
- pyroxide hydrochloride (improves metabolism, necessary for the normal functioning of the central and peripheral nervous system);
- nootropic drugs (intended for a specific effect on the psyche);
- glucocorticosteroid drugs (have anti-inflammatory, desensitizing, immunosuppressive, antishock and antitoxic effects);
- antibiotic therapy (helps fight bacterial infections).
In some cases, it is possible to use other drugs as prescribed by the doctor. Warming the patient is sometimes used.
Opioids in history
Humanity knew what opioids were 4 thousand years ago. It is known that in the Minoan civilization a goddess was especially revered, whose image was surrounded by a crown of opium poppy pods. Opioids were also known to later civilizations - Corinth (Greece) and Afyon (Turkey). From there, the extraction of opium from poppies spread to the East.
It should be noted that until the middle of the 17th century, opioids were used exclusively as a painkiller, and not as a drug. But smoking opium in the desire to fall into euphoria began to spread in China in the second half of the 17th century. One cannot help but recall the so-called Opium Wars, which broke out at the end of the 18th century. The reason for this was that the British East India Company, taking advantage of its monopoly position, imported huge amounts of opium into China.
Further, the history of drugs and opioid drugs developed as follows:
- 1804 - the German pharmacist F. Serturner was able to extract its main active ingredient from opium, which the discoverer called “morphine” (the term “morphine” was introduced somewhat later by Gay-Lussac).
- 1898 - semi-synthetic derivatives of morphine, called “heroin” and “ethylmorphine”, came into medical use.
- 1937 - The first fully synthetic opioid pethidine was produced in Germany. A little later, methadone of the same nature was synthesized. In the Soviet Union, a derivative of pethidine, promedol, was used.
- Late 1950s - Fentanyl was synthesized in Belgium.
Possible complications
Unfortunately, opiate poisoning leads to negative consequences. Severe complications include:
- postanoxic encephalopathy - impaired blood circulation in the brain;
- paralysis and paresis - disruptions in neurological functions, difficulty moving muscles;
- affective states – changes in mental state;
- pneumonia (aspiration, inhalation) – inflammation of the lung tissue;
- acute kidney injury.
Other unhealthy manifestations are also possible. They are quite dangerous and require immediate medical attention. The most severe form of consequences can be drug addiction, which will occur in four stages:
- uncontrollable desire to buy and use drugs;
- physical and mental need to increase the dose over time;
- formation of stable dependence on opiates;
- intense degradation of a person as an individual.
If immediate measures are not taken to treat drug cravings, death occurs.
Negative effects of opioids
The main disadvantage of the drug is the emergence of dependence on opioids. The following follows from this:
- Strong narcotic desire to use the drug.
- Impaired ability to control one's behavior.
- The appearance of harmful consequences.
- Losing the meaning of normal life in pursuit of the effect of an opioid.
- Withdrawal after stopping the use of the medicine.
Addiction and its consequences can arise both after long-term use of opioid painkillers with a doctor’s prescription (for example, in the case of severe chronic pain), and as a result of illegal diversion of the drug from the warehouses of enterprises, pharmacies, and medical institutions. Nowadays, effective measures to combat it have been developed.
How does intoxication manifest itself at different stages?
The effect of opiates: the face turns red, there is a feeling of warmth in the lower back and abdomen, the addict is focused on his fantasies. In acute poisoning with opium narcotic substances, the sensations are different. The toxicogenic stage is manifested by a triad of characteristic signs: depression of consciousness (stupor), pronounced constriction of the pupils, respiratory failure (bradypnea). Other symptoms quickly follow:
- decrease in temperature;
- vomiting (aspiration of vomit is dangerous);
- convulsions;
- disturbance of urination and defecation (delay);
- rhabdomyolysis (muscle dysfunction);
- pyrogenic reactions (fever, chills, headache).
External manifestations of poisoning are accompanied by serious disturbances in the activity of the central nervous system and brain. Encephalopathy develops, and toxic cerebral edema and pulmonary edema may develop. Myocardial damage associated with hypoxia provokes cardiovascular failure, including cardiac arrest. There are 4 phases of acute opiate poisoning:
- Stage 1 (mild degree of poisoning).
The patient is communicative, but is in a state of deafness, speech is inhibited. The reaction to light is reduced or absent, oculomotor disturbances (nystagmus, ptosis) are noted. There is respiratory distress, pain sensitivity is weakened, and the pulse is rare.
- Stage 2 (moderate condition) – phase of superficial coma.
Characterized by a lack of consciousness in the patient. The skin is pale, there is no reaction to light and external stimuli, tendon reflexes are preserved. Cyanosis, central respiratory depression), a drop in blood pressure, and convulsions are noted.
- Stage 3 (very severe condition) – deep coma phase.
Consciousness, reactions, sensitivity, reflexes are absent. Severe respiratory depression, cyanosis, hemodynamic disturbances. Brain swelling develops, and breathing may stop. Without timely assistance, about 80% of patients die after 5–10 hours.
- Stage 4 – the patient comes out of the coma.
This phase occurs when the dosage of opiates is slightly exceeded or during chronic intoxication. The functions of the body are restored independently: breathing is normalized, blood circulation is restored, consciousness returns.
Signs of withdrawal syndrome
After the onset of the somatogenic stage (when toxins are eliminated from the body), the patient may experience signs of withdrawal syndrome, that is, abstinence syndrome. Signs of withdrawal and their severity depend on the “experience” of drug addiction and on how long the addict was deprived of the usual dose of opium drugs.
The first phase develops 10–12 hours after the “overdose”. It is characterized by manifestations of physical dependence, as well as vegetative signs: dilated pupils are noted, the patient often yawns, and his eyes water. There is no appetite, sleep is disturbed. In the second phase, chills, sweating, a feeling of heat, lacrimation and drooling appear. The muscles are tense, painful, the patient yawns intensely and sneezes.
By the end of the second day of opium withdrawal, the third phase begins - it is characterized by severe muscle pain and cramps. The person is tense, cannot sit still, and depression appears. The fourth phase develops the next day: the listed manifestations are joined by dyspepsia, vomiting, skin itching, the temperature rises, and the pulse increases greatly.
Diagnostics
Diagnosis of acute opium poisoning is based on medical history (if possible), the specificity of the clinical picture, as well as laboratory data. Thanks to tests, the doctor can determine which drug caused the poisoning. If 6-mono-acetylmorphine is detected in the blood, this indicates the use of an opiate such as heroin. Morphine can be detected in urine after two days, codeine - within three days.
An antidote is often used to diagnose opiate poisoning - usually Naloxone, an opiate antagonist. The doctor analyzes the patient’s condition (the size of the pupils, how much consciousness is depressed, what is the respiratory rate) before and after applying the antidote. If a reaction occurs to the administration of the drug, this speaks in favor of opium poisoning. All changes and results of toxic-chemical studies must be recorded in detail in the medical history. This is important both for making a correct diagnosis and for determining the effectiveness of therapy for poisoning.
Prescribing an opioid analgesic
The attending physician has the right to prescribe such a controversial drug as an opioid analgesic in the following cases:
- The use of other types of analgesics does not bring the desired effect. This is typical, for example, for cancer patients suffering from chronic severe pain, which is why they are prescribed opioid agonists.
- According to the pain scale, the patient's syndrome goes beyond the level of mild pain (4 - the most severe, 3 - severe, 2 - moderate, 1 - weak, 0 - not present). So, for example, in Russia: for o: fentanyl, morphine;
- for o: buprenorphine;
- for about: prosidol, tramadol.
Separation by impact
What are these opioid drugs? These are also means that are divided according to the intensity of their impact on the systems of the human body. Within this framework, three groups are distinguished:
- Potent drugs: fentanyl, buprenorphine, sufentanil, carfentanil, remifentanil, brifentanil, alfentanil.
- Medium intensity drugs: pentazocine, codeine, trimeperidine, nalbuphine.
- Weak drugs - for example, tramadol.
Marijuana: buds, hashish, oil
In most cases, all symptoms are short-lived and do not pose any danger. There have been no recorded deaths caused by marijuana use.
During an attack of fear, panic or paranoia
We must try not to think about the exciting question and switch to another thought. Eat something sweet (it will reduce the effect of marijuana), such as a mint candy. You can take Corvalol, up to 30 drops (only with severe fear that does not go away for a long time).
For extreme agitation, confusion, or severe hallucinations
Such situations are extremely rare. If it does arise, you must try to calm the person down. You can give him a placebo - any vitamin (watch carefully what you give!), and tell him that this pill will “immediately and gradually begin to go away.” You can take a couple of breaths of ammonia (ammonia), which is in every car first aid kit, or rub it on your temples.
With rapid heartbeat or high blood pressure
You need to try to calm down, wash your face with cold water, drink and eat sweets. Help is needed only if problems are obvious (monitor symptoms).